 Peptide synthesis
Peptide synthesis
Are peptide vaccines providing a safer and more cost-effective alternative to conventional vaccines in protecting against life-threatening and chronic diseases?
Vaccines are often considered the most successful medical treatment of the past centuries. They were designed to leverage our immune system and produce long-lasting protection against specific diseases. Conventional vaccines have relied on the use of inactive pathogens to elicit an immune response. However, many of these formulations have a high risk of causing allergic or autoimmune responses. Peptide vaccines are increasingly being regarded as a cost-effective and safe way to circumvent this problem.
Conventional vs peptide vaccines
Modern vaccination strategies may have been popularized after the development of the first smallpox vaccine by Edward Jenner in 1796. Nonetheless, there are historical evidences that vaccines were being used in Asia and Africa long before that.
Despite the centuries-old techniques, it was Jenner’s discovery that administering cowpox to human patients could prevent the spread of smallpox with minimal side effects. This approach prompted the development of scalable vaccination strategies that are continuously being improved in an attempt to eradicate life-threatening diseases.
Conventional infection-targeting vaccines have relied on the use of attenuated or inactivated forms of pathogens or components thereof. These classical formulations usually contain up to hundreds of different proteins, but only a small fraction of these will be responsible for inducing a proper protective response.
Whole-pathogen-based formulations are still recurrently used. These vaccines are effective because they contain the entire disease-causing agent and produce long-lasting immunity against it.
Yet, there are many disadvantages to using whole-pathogen formulations.
For instance, recent studies show that many times, allergic or autoimmune reactions can originate from common contaminants present in these formulations. This happens because pathogens are grown in standard culture medium containing antibiotics and biological residues. These residues are not fully removed after the inactivation of the pathogen and they often result in a strong allergic reaction when administered to patients.
Also, the attenuated or inactivated pathogen may return to its virulent state, which further endangers patients, medical staff and workers responsible for vaccine production.
Moreover, the use of whole-pathogen approaches is often unfeasible due to the inherent difficulties of culturing certain pathogens under standard laboratory conditions (e.g. intracellular pathogens).
With the development of recombinant technologies, vaccines quickly evolved to adopt protein-based approaches. But even single proteins may be hard and expensive to produce. Also, these proteins contain many unspecific epitopes that elicit a weak immune response. In addition to these problems, these biomolecules are regularly produced by recombinant microorganisms which adds difficulty to the subsequent purification process and increases the risk of allergenic contaminations.
These drawbacks led scientists on the search for the minimal immunogenic peptide sequence, which resulted in the discovery of peptide vaccines.
Advantages and limitations of peptide vaccines
Peptide vaccines are often portrayed as the most promising tendency in vaccine development.
But the use of peptides for immunization is not a new concept.
The first synthetic peptide vaccine was reported by scientists from the Institute for Animal Science and Health in The Netherlands in 1994. But researchers had been using immunogenic peptides since the 1980s for the in vivo generation of epitope-specific antibodies, also known as peptide antibodies.
The use of peptides allows vaccines to target very specific epitopes while minimizing the risks of allergic or autoimmune reactions. But besides the advantages in terms of specificity and safety, the use of peptides as immunogens also offers interesting advantages by lowering vaccine’s production costs and lead times.
Nevertheless, developing vaccines based on these minimal sequences is not without its challenges.
Peptides often lack immunogenicity and, for this reason, they frequently fail to induce an effective immune response. Besides, these molecules are very unstable on our organism, as they can be easily degraded by widespread proteases long before they succeed at eliciting an immune response.
For the past decades, scientists have devised countless strategies to overcome these limitations. Conjugation has been one of the most successful strategies developed to date.
For instance, peptides can be conjugated with proteins (e.g. KLH or BSA). These groups help to increase their stability and immunogenicity. Nevertheless, they also increase the risks of provoking unwanted allergic responses. Unsurprisingly, these groups may also induce conformational changes to the peptides, rendering these peptide-based vaccines ineffective. For these reasons, the conjugation of peptides needs to be carefully considered to avoid these drawbacks.
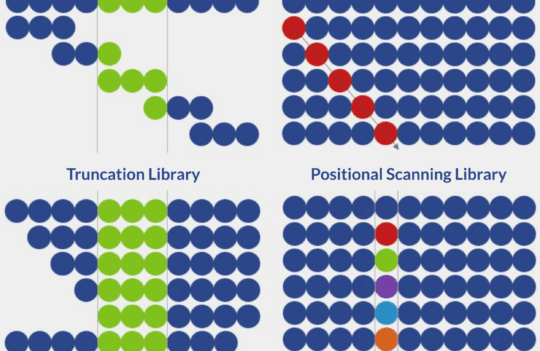
Another suitable alternative to increase peptide stability and immunogenicity relies on the development of multimeric peptide vaccines.
The proof-of-concept has been proposed by researchers from Rockefeller University as early as 1988. Their solution consisted of using several linked copies of an antigen to elicit a stronger immune response. Afterward, several studies from independent groups have consistently showed that the use of multiple copies of a peptide targeting the same epitope or a combination of different epitopes against the same antigen is more efficient than the use of the unconjugated peptide itself.
Summary of the key features of peptide vaccines
- Peptide vaccines can be exclusively produced using chemical synthesis, such as solid-phase peptide synthesis approaches
- Suitable for large-scale and cost-effective production
- Formulations are free from biological contaminating material, often known to cause allergic or autoimmune responses
- The use of peptides can modulate the immune response by designing the vaccines to target very specific domains
- Peptides can be easily modified (i.e. with lipids, carbohydrates, phosphate, acetyl and amide groups) to increase stability, immunogenicity, and solubility
Challenges in the development of anti-infective peptide vaccines
Traditionally, vaccines have been used to protect against viral and bacterial infections. Interestingly, greater challenges have been found in the development of antifungal therapies.
This is especially worrisome because fungi are still considered a major cause of mortality around the world. The eradication of invasive fungal infections usually requires months to years of continuous administration, often leading to an exacerbated risk of selecting for drug-resistant variants which may perpetuate the infection.
Additionally, many emerging fungal diseases are caused by multidrug-resistant fungal strains, such as Candida auris, first reported in 2009. Besides these obstacles, there is a limited amount of antifungal drugs approved for therapy and many of them are known to cause severe side-effects on patients.
The high incidence of drug resistance and the inherent toxicity of antifungal drugs has led to an increased interest in the development of antifungal vaccines. However, the genetic complexity of fungal cells continues to present multiple challenges. For instance, scientists still don’t fully understand the antifungal humoral immune response and thus, it is hard to identify and select suitable epitopes or even antigens for adequate vaccination strategies.
Nevertheless, recent studies with Sporothrix brasiliensis, a fungal disease endemic in Rio de Janeiro (Brazil) showed promising results. Researchers from the University of Sao Paulo found that mice immunized with specific peptides were more likely to survive when challenged with S. brasiliensis. But more studies are necessary to further understand which antigens provide the strongest protective reaction.
Concluding remarks
The search for the minimal immunogenic sequence has led to a new generation of vaccines called peptide vaccines. Many researchers consider these vaccines the future of human and animal immunization.
Peptide vaccines have the advantage of reducing production costs and considerably reducing the risks of allergic and autoimmune responses while maintaining the ability to protect patients against life-threatening illnesses.
Yet, it is still especially challenging to develop suitable peptide vaccines. This happens because many of these minimal peptide sequences cannot induce an efficient immune response by themselves.
Many researchers have proposed conjugation with other molecules and other epitopes of the same disease as a way to circumvent this problem. This rationale continues to prompt the development of many of these vaccines to alleviate the burden of many diseases.
- de Almeida, J. R. F. et al. An immunoproteomic approach revealing peptides from Sporothrix brasiliensis that induce a cellular immune response in subcutaneous sporotrichosis. Sci Rep. 2018; 8(1):4192. doi: 10.1038/s41598-018-22709-8
- Langeveld, J. P. et al. First peptide vaccine providing protection against viral infection in the target animal: studies of canine parvovirus in dogs. J Virol. 1994; 68(7):4506-4513. Available from https://www.ncbi.nlm.nih.gov/pubmed/8207825
- Li, W. et al. Peptide Vaccine: Progress and Challenges. Vaccines (Basel). 2014; 2(3):515–536. doi: 10.3390/vaccines2030515
- Skwarczynski, M. and Toth, I. Peptide-based synthetic vaccines. Chem Sci. 2016; 7(2): 842–854. doi: 10.1039/c5sc03892h
- Taborda, C. P. and Nosanchuk, J. D. Editorial: Vaccines, Immunotherapy and New Antifungal Therapy against Fungi: Updates in the New Frontier. Front Microbiol. 2017; 8:1743. doi: 10.3389/fmicb.2017.01743