Antibody production
Antibody production
Challenges and considerations in primary antibody production for medical imaging
The term primary antibody is commonly used to describe antigen-binding antibodies with use for research and diagnostics. However, primary antibodies used for medical imaging are special. Besides requiring low toxicity and antigenicity, they also need to be able to persist in the human organism for long enough to reach their target. Interestingly, clinical researchers are increasingly aware that these antibodies may actually hold the key to understand why many immunotherapies fail.
Primary antibody production for medical imaging
Primary antibodies are designed to bind to specific antigens. Their purpose is to detect, purify or measure specific molecules, which makes them important tools for research and diagnostics.
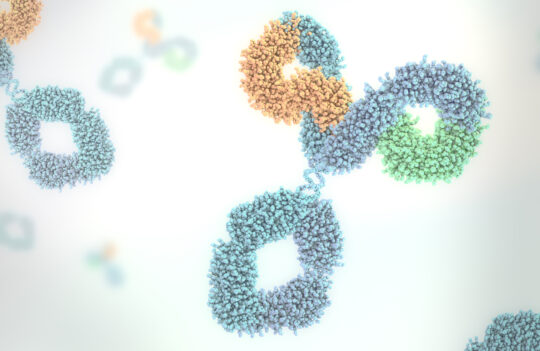
These molecules can be used alone, or in combination with a secondary antibody (binds to the primary antibody). When assays employ only primary antibodies, they are referred to as direct detection assays. On the contrary, when assays combine the use of unlabeled primary antibodies and labeled secondary antibodies, they allow indirect detection of an antigen, which results in signal amplification.
Indirect detection can be advantageous for certain analytical applications, especially when the antigen is found in low abundance. However, when antibodies are used as imaging agents, direct labeling is the most obvious solution as the antibody needs to enter the organism, persist long enough to reach its target, and diffuse across tissues.
Interestingly, imaging agents, need to fulfill certain requirements regarding safety. Like therapeutic antibodies, these agents need to have certain properties including low toxicity and antigenicity, and good biodistribution and pharmacokinetics in the organism.
Thus, primary antibody production for imaging is not much different from therapeutic antibody production.
In this context, different approaches can be considered for primary antibody production:
- Antibody generation stage: hybridoma (in vivo) or phage display technologies (in vitro)
- Antibody production stage: cell culture supernatant, or recombinant production
Traditionally, antibodies have been generated in vivo using animal hosts and the hybridoma technology. This mature technology allows the generation of antibodies with a high affinity towards specific targets. Nevertheless, these molecules find limited application for therapy and imaging in humans, as their low compatibility with the human immune system often causes allergic responses and limits their effectiveness in the long term.
Thus, primary antibody production, similar to therapeutic antibody production, is increasingly generated in vitro (e.g. phage display) and subsequently produced by recombinant technologies. Contrary to the hybridoma technology, in vitro generation allows the production of fully human antibodies, minimizing adverse and allergic reactions.
Redefining primary antibody production to understand the challenges of new immunotherapies
In 2017, Rosie Metsel published an article in Nature on the advantages of harnessing imaging immunotechnologies for preclinical and clinical research.
As Metsel pointed out, one of the most important bottlenecks against the implementation of life-saving immunotherapies arises from our lack of knowledge of how these drugs act in our organism.
Most drugs end up failing preclinical and clinical trials due to unforeseen interactions between the foreign molecule and our organism. And, for the most part, we’re still unable to understand the reasons behind these failures.
For this to change, we need to understand what happens once these molecules enter our organism.
One technology with the power to allow us a glimpse into what happens in our organism during immunotherapy is immunoPET.
ImmunoPET, also known as immuno–positron emission tomography, combines PET with monoclonal antibodies to improve tumor diagnosis and characterization. This technique, first described by scientists from the VU University Medical Center (The Netherlands), allows researchers and physicians to map the tumor’s exact location and size in real-time.
In its essence, it enables in vivo immunohistochemical staining and, thus, can be used to visualize and monitor the evolution of specific tumors using a full-body PET scan.
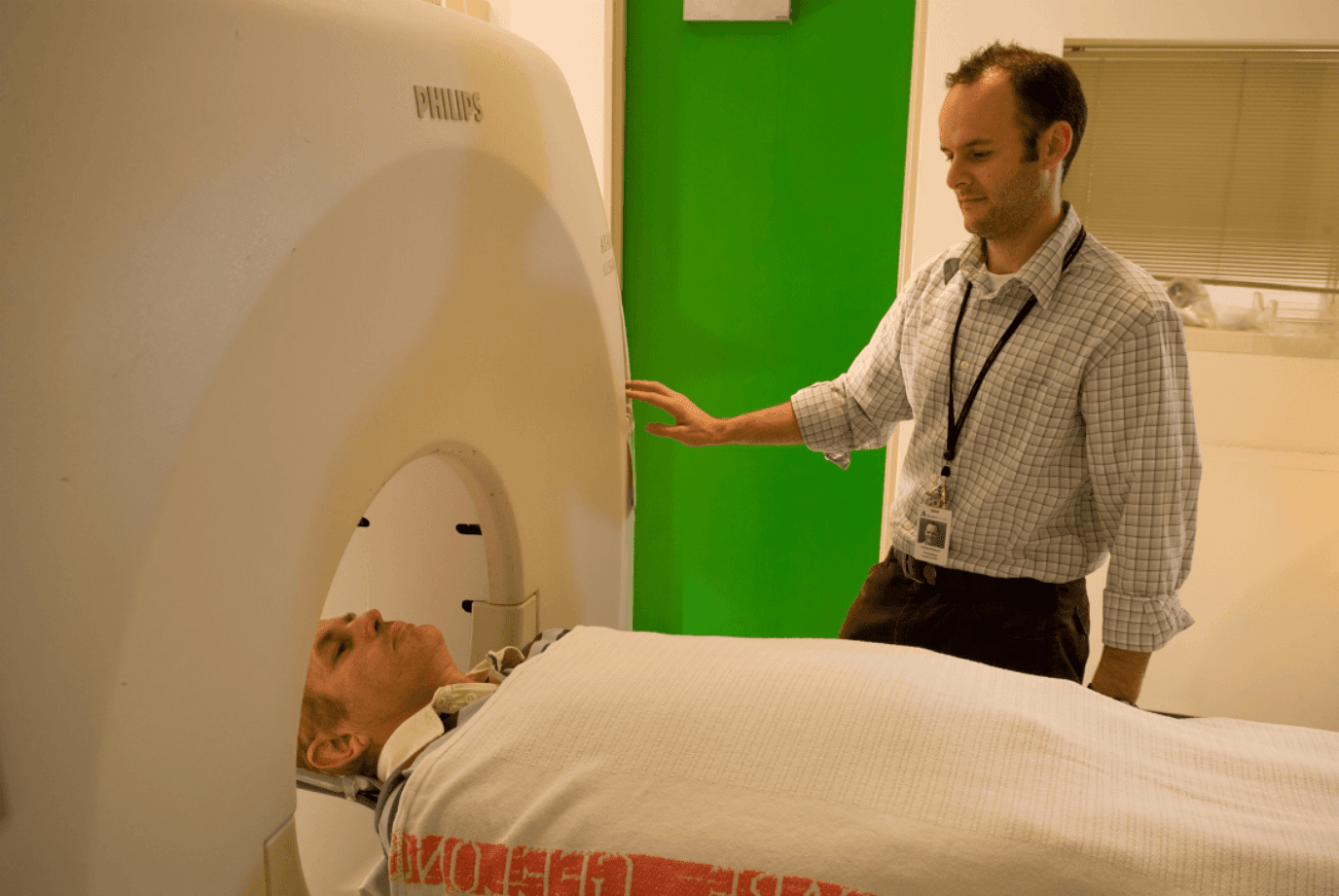
For this to work, antibodies are labeled with short-lived radioactive isotopes (e.g. zirconium-89 or iodine-124) that emit positrons. When these positrons lose their kinetic energy and collide with electrons in our organism, they immediately produce two γ photons and emit them in opposite directions.
The detection of these photons and subsequent overlay of data, allows researchers to determine the label’s initial position.
Researchers are already using this technology to understand why patients respond differently to cancer immunotherapies.
For instance, in 2016 scientists from the University Medical Center (The Netherlands) studied the response of breast cancer patients to Kadcyla treatment (trastuzumab emtansine, Drug Bank accession number DB05773). This drug, a conjugate between an anti-cancer monoclonal antibody and the cytotoxic drug DM1, binds to the tumor protein HER2.
Using radioactive labeling, researchers found that tumors didn’t uptake the drug in at least 29% of the patients. This explained why the treatment was failing in some cases.
The team is confident that studying the reasons for this behavior could help clinicians make more informed decisions on anti-cancer treatments and also aid researchers in designing better drugs.
Alternatives to increase the efficiency of current immunoPET technologies
Traditionally, immunoPET was designed to be used with monoclonal antibodies and short-lived radioactive isotopes. These primary molecules are stable, robust and have long half-lives in our organism. However, they can also take up to a week to reach their target and be cleared out from the body.
Thus, the patient needs to be exposed to radiation during the time it takes the conjugate to reach its intended target.
A strategy to reduce the exposure to radiation relies on a two-step approach. Instead of putting the radioactive label in the antibody, researchers suggest injecting the unlabeled antibody, waiting one week for the unbound molecule to clear the organism, and then injecting a smaller radiolabeled probe.
This approach, commonly known as pre-targeted imaging, relies on the use of bispecific antibodies with the ability to bind two different targets: the antigen and the radiolabeled probe (also called a hapten).
Successful pre-targeting strategies commonly use peptide-based or chelate-based haptens. Some of these approaches showed promising results during preclinical trials. However, to date, none of these molecules was granted approval for clinical use.
Despite decreasing the exposure, this strategy fails to reduce the one-week timeframe imposed by the conventional immunoPET analysis. That timeframe may be acceptable during preclinical or clinical studies, however, for patients facing the risk of metastatic cancer, early detection could prolong or even save their lives.
A solution to this problem involved the use of smaller molecules, such as nanobodies or antibody fragments, instead of monoclonal antibodies. Nanobodies present an interesting solution due to their small size, stability, high affinity, and good solubility. However, as several preclinical studies pointed out, these proteins often clear too quickly from our organism to be suitable agents for PET-based applications.
To circumvent this problem, many researchers suggest coupling nanobodies with polyethylene glycol (PEG), albumin or Fc fragments. Nevertheless, to date, we lack solid evidence regarding the effectiveness of these approaches in mitigating the inherent limitation of nanobodies and reducing the timeframe of immunoPET imaging.
Concluding remarks
Primary antibody production needs to be tailored to the specific constraints and requirements of every application. For instance, for medical imaging, these antibodies need to show reduced antigenicity and, at the same time, a slow clearance from the organism.
Medical imaging, based on immunoPET has shown promising results with application to diagnostics and clinical research. However, to this date, none of these diagnostic and monitoring tools has been granted approval for clinical use.
- van Dongen, G. A. M. S. et al. Immuno-PET: A Navigator in Monoclonal Antibody Development and Applications. Oncologist. 2007; 12(12):1379-1389. doi: 10.1634/theoncologist
- den Hollander, M. W. et al. TGF-β Antibody Uptake in Recurrent High-Grade Glioma Imaged with 89Zr-Fresolimumab PET. J Nucl Med. 2015; 56(9): 1310-1314. doi: 10.2967/jnumed.115
- Gebhart, G. et al. Molecular imaging as a tool to investigate heterogeneity of advanced HER2-positive breast cancer and to predict patient outcome under trastuzumab emtansine (T-DM1): the ZEPHIR trial. Ann Oncol. 2016; 27(4):619-624. doi: 10.1093/annonc/mdv577
- Lecocq, Q. et al. Theranostics in immuno-oncology using nanobody derivatives. Theranostics. 2019; 9(25): 7772-7791. doi:10.7150/thno.34941
- Mestel, R. Cancer: Imaging with antibodies. Nature. 2017; 543:743-746. doi: 10.1038/543743a
- Reddy, S. and Robinson, M. ImmunoPET In Cancer Models. Semin Nucl Med. 2010; 40(3): 182–189. doi: 10.1053/j.semnuclmed.2009.12.004
- Vaidyanathan, G. et al. Preclinical Evaluation of 18F-Labeled Anti-HER2 Nanobody Conjugates for Imaging HER2 Receptor Expression by ImmunoPET. J Nucl Med. 2016; 57(6): 967–973. doi: 10.2967/jnumed.115.171306
- Verel, I. et al. The Promise of Immuno-PET in Radioimmunotherapy. J Nucl Med. 2005; 46 Suppl 1:164S-171S. Available from http://jnm.snmjournals.org/content/46/1_suppl/164S.long