 Antibody production
Antibody production
Antibody production: hybridoma technology as the preferred method for therapeutic applications?
Up to 2019, 79 antibodies were granted approval by the FDA or EMA for clinical use in the US or EU, respectively. 48 of these 79 antibodies were generated and developed using hybridoma technologies. Notably, the 6 antibodies approved for clinical use in 2019 were all generated using this robust in vivo approach. The high approval rate shows that hybridoma production for therapeutic applications continues to be an indisputable technology for drug discovery.
Will antibody production in hybridomas still be relevant in the 2020s?
Despite the fact that 2019 ended with an unusually low amount of clinical approvals, the year didn’t fail to bring some notable successes. For instance, among the 6 antibodies approved in 2019, Brolucizumab represents the most significant achievement. Sponsored by Novartis, Brolucizumab was obtained by humanizing rabbit hybridomas, becoming thus the first hybridoma-derived antibody to be developed in a species other than mice.
Its success brings a renewed interest to antibody production in hybridomas. More interestingly, it continues to prompt researchers and industry leaders to further develop this technology.
Phage display and in vivo antibody generation in transgenic mice are the two other dominant technologies in therapeutic antibody discovery. Nevertheless, the advantage of hybridomas in comparison to the other techniques is clearly defined.
Hybridoma-derived antibodies offer unique advantages. For instance, in comparison to the phage display technology, hybridomas allow the conservation of the natural pairing information between heavy and light chains. This natural pairing information can thus be used to adapt these molecules for recombinant production, ensuring the highest stability and in vivo efficiency of these biopharmaceuticals. Moreover, these antibodies are generated in vivo, which ensures an optimal and cost-effective process of affinity maturation.
The advantages of hybridomas over antibody generation in transgenic mice are quite different. For instance, unlike transgenic mice, hybridomas are not generally protected by patents, with the notable exception of rabbit hybridomas. For this reason, this continues to ensure the fast progress and optimization of the technology.
Moreover, unlike the hybridoma technology, the production of human antibodies in transgenic animals is restricted to mice-like antibodies. Although mice-derived antibodies have been crucial for the development of many immunotherapies, currently, there is a considerable shift towards other types of antibodies, such as rabbit and camelid heavy-chain antibodies, characterized by higher stability and affinity.
Challenges and limitations of antibody production in hybridomas
Noticeably, there are still considerable time and technical constraints tied to antibody production in hybridomas. Specifically, it may take between 4 to 6 months to develop a new hybridoma cell line, and more than 5 months to humanize the xenogeneic antibody and subsequently ensure its therapeutic efficiency. This effort implies the use of time-consuming engineering techniques and the optimization of antibody expression in recombinant systems.
Moreover, the stable generation of hybridomas is still confined to a small number of species.
This constraint derives from the need to produce stable and optimized myeloma fusion partners for each specific species. To date, only a restricted number of species have established fusion partners which were typically obtained from myeloma cells isolated and subsequently adapted and optimized for fusion from the same host.
For this reason, to date, hybridomas have only successfully been reported for mouse, human, and rabbit. Moreover, from these species, only mouse and rabbit hybridomas are used at a commercial and industrial level.
Future approaches for antibody production in hybridomas
The hybridoma technology currently faces three main challenges:
- The reduced availability of optimal myeloma fusion partners for B cells isolated from nonmodel species or lack of more efficient techniques for the immortalization of B cells
- The still reduced efficiency of current cell fusion techniques
- The reduced scalability of current hybridoma screening methodologies.
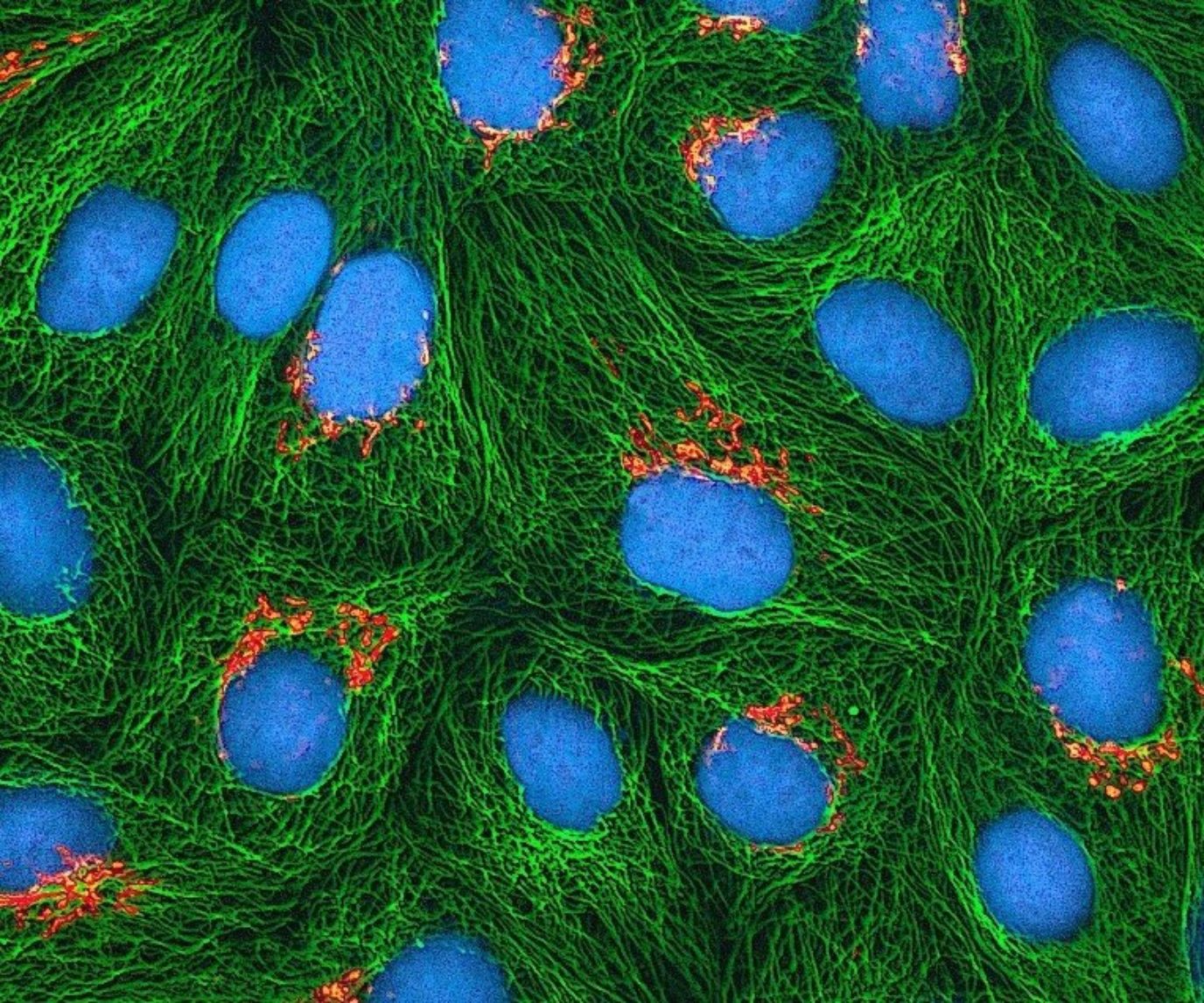
For many decades, cell fusion between antibody-secreting B cells and myelomas has been the preferred approach for the immortalization and stabilization of antibody-secreting B cells. Although earlier works have focused on B cell immortalization using Epstein-Barr virus (EBV), the efficiency of this approach is limited.
Thus, current immortalization of B cells relies on the fusion with myeloma partner using either viral, PEG, electrofusion, or laser fusion methods with varying degrees of success. Today, PEG-mediated cell fusion continues to be the preferred method for creating antibody-secreting immortal cell lines.
Nevertheless, most of these techniques have remained largely unchanged for the last 20 years. And literature concerning the improvement of current hybridoma platforms has since become scarce. Notably, Tim Steele, a researcher from the University of Maryland University College (US), published a review in 2016 addressing the current limitations and trends in hybridoma development.
In this review, he identified the progressive development of microfluidics and single-cell screening and sequencing technologies as the two approaches with the power to leverage and reinvent antibody production in hybridomas. However, to this date, only a few studies reported the successful use of single-cell microfluidic-based technologies for screening and identifying specific antibody-producing hybridomas or B cells from heterogeneous populations.
Concluding remarks
Antibody production in hybridomas has led to the generation of countless invaluable biotherapeutics. To date, more than 60% of all antibodies approved for clinical use were produced using the hybridoma platform. Interestingly, all antibodies approved in 2019 were obtained using these mature and robust technologies.
Nevertheless, many experts are currently attempting to reinvent this technology by leveraging the screening power of current microfluidics and single-cell technologies. These will likely drive the progress in antibody discovery in countless new species.
- Debs, B. E. et al. Functional single-cell hybridoma screening using droplet-based microfluidics. Proc Natl Acad Sci U S A. 2012; 109(29):11570-11575. doi: 10.1073/pnas.1204514109
- Seah, Y. F. S. et al. Microfluidic single-cell technology in immunology and antibody screening. Mol Aspects Med. 2018; 59:47-61. doi: 10.1016/j.mam.2017.09.004
- Steele, T. Life begins at forty – hybridomas: ageing technology holds promise for future drug discoveries. GaBI Journal. 2016; 5(1):21-26. doi: 10.5639/gabij.2016.0501.006