 Antibody-drug conjugates
Antibody-drug conjugates
Antibody-antibiotic conjugates for therapeutic applications
Antibody-antibiotic conjugates (AACs) are an emerging class of biotherapeutics for the treatment of infectious diseases. With the rise of antibiotic resistance, this new class of drugs is expected to gain ground over conventional therapeutic strategies within the next decades. In this article, we discuss the state-of-the-art of this field, the advantages of using antibiotics as payloads of ADCs, and provide clues regarding future trends.
Advantages of antibody-antibiotic conjugates
Antibiotics are considered the hallmark of modern medicine. For decades, they have helped control outbreaks of infectious diseases and allowed the safe practice of invasive surgery. However, in recent years, the rise of antibiotic resistance and multi-drug resistance accompanied by the decline in the discovery and development of novel antibiotics have led to a worldwide crisis that, if unsolved, could have devastating consequences.
The use of monoclonal antibodies or antibody-drug conjugates (ADCs) has found great success in the treatment of complex diseases such as cancer and autoimmune disorders. However, the efficacy of these therapies has been limited when targeting infectious diseases. To overcome this limitation and counter the crisis brought by the rise of antibiotic resistance, antibody-antibiotic conjugates (AACs) were recently proposed as an alternative treatment.
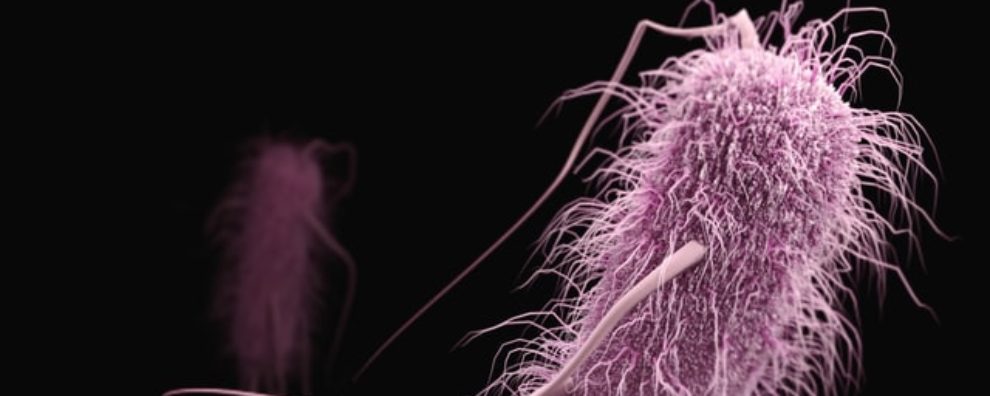
AACs combine the specificity and long plasma half-life of antibodies with the antimicrobial activity of antibiotics. Although these combination therapies have yet to reach the market, AACs already proved to be effective in the treatment of Staphylococcus aureus bacteremia. Experts agree that these therapies will help control the development of antibiotic resistance by ensuring these therapies target only a subset of the entire human microbiota. Moreover, this novel methodology will further allow the use of antibiotic classes previously abandoned due to high toxicity or unfavorable pharmacokinetics.
The example of RG7861, an anti-S. aureus AAC
The most well-documented and cited case of a successful AAC is that of RG7861, developed by Genentech using the THIOMAB™ technology and designed to target intracellular S. aureus. The conjugate consists of a human monoclonal antibody targeting wall teichoic acid (WTA) coupled to the rifalazil analog – dmDNA31 or rifalog (dimethyl DNA31, 4-dimethylamino piperidino-hydroxybenzoxazinorifamycin) via a cathepsin cleavable linker (modified valine-citrulline linker).
The conjugate has demonstrated a favorable safety and pharmacokinetic profile in phase I clinical trials. It promises to become one of the first treatments of its kind to receive marketing authorization by the FDA.
What makes this treatment so promising is the increasing clinical prevalence of S. aureus infections. After Clostridium difficile, S. aureus is one of the most frequently reported hospital-acquired infections and the most common pathogen found in patients with ventilator-associated pneumonia. These infections have been increasingly difficult to treat due to the emergence of methicillin-resistant S. aureus (MRSA), which severely limited the use of vancomycin, an antibiotic that has historically been highly successful against this pathogen. In addition to these factors, S. aureus strains are notoriously hard to eliminate due to their ability to survive and persist inside host cells (i.e., neutrophils and dendritic cells).
The ability to target pathogens intracellularly has so far only been possible when using combination therapies such as AACs. These biotherapeutics can bind to the surface-exposed WTA in S. aureus, when the complex formed by the pathogen and the AAC are internalized by host cells, the protease-cleavable linker is degraded leading to the release of the antibiotic in the intracellular environment. Rifalog is a potent RNA polymerase inhibitor able to act on persisters (dormant cells) and stationary-phase S. aureus cells.
Therapeutic potential of AACs for treating infectious diseases
The preliminary results obtained with RG7861 will serve as the basis for the development of new AAC therapies. However, it is important to recognize that the conjugation with antibodies considerably increases the cost of antimicrobial therapies. For this reason, experts recommend focusing on the generation of AACs to target hard-to-treat infections such as tuberculosis, a leading cause of death worldwide.
These emerging biotherapeutics can also be used to mitigate the adverse effects of broad-spectrum antibiotics. These therapies, although highly effective, are known to target both pathogens and commensal bacteria in a non-discriminating way. By coupling them with target-specific antibodies, it is possible to reduce the damage caused by these agents to gut microbiota.
This is particularly useful when targeting bacterial biofilms (highly persistent aggregates consisting of dormant or stationary phase cells, naturally resistant to many antibiotics), that require high local doses of antimicrobials to be eliminated.
However, the most important drawback of these therapies is the need to increase the drug-to-antibody ratio (DAR). Current therapies can accommodate 2 antibiotic molecules. But because these drugs are considerably less toxic than the drugs used in conventional ADC development, it is urgent that AACs can carry a significantly higher number of antibiotics.
- Mariathasan, S. and Tan, M. W. Antibody-Antibiotic Conjugates: A Novel Therapeutic Platform against Bacterial Infections. Trends Mol Med. 2017; 23(2):135-149. doi: 10.1016/j.molmed.2016.12.008
- Peck, M. et al. A Phase 1, Randomized, Single-Ascending-Dose Study To Investigate the Safety, Tolerability, and Pharmacokinetics of DSTA4637S, an Anti-Staphylococcus aureus Thiomab Antibody-Antibiotic Conjugate, in Healthy Volunteers. Antimicrob Agents Chemother. 2019; 63(6): e02588-18. doi: 10.1128/AAC.02588-18