Antibody production
Antibody production
“Researchers are not leveraging the speed and resolution of flow cytometry for clinical evaluation”
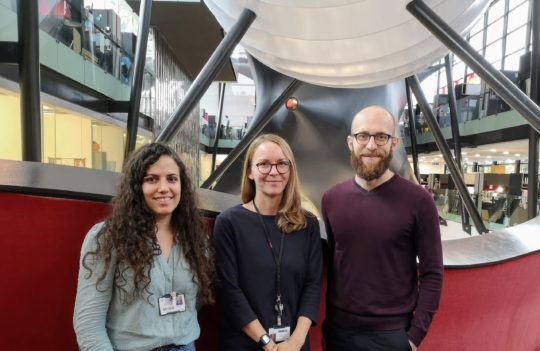
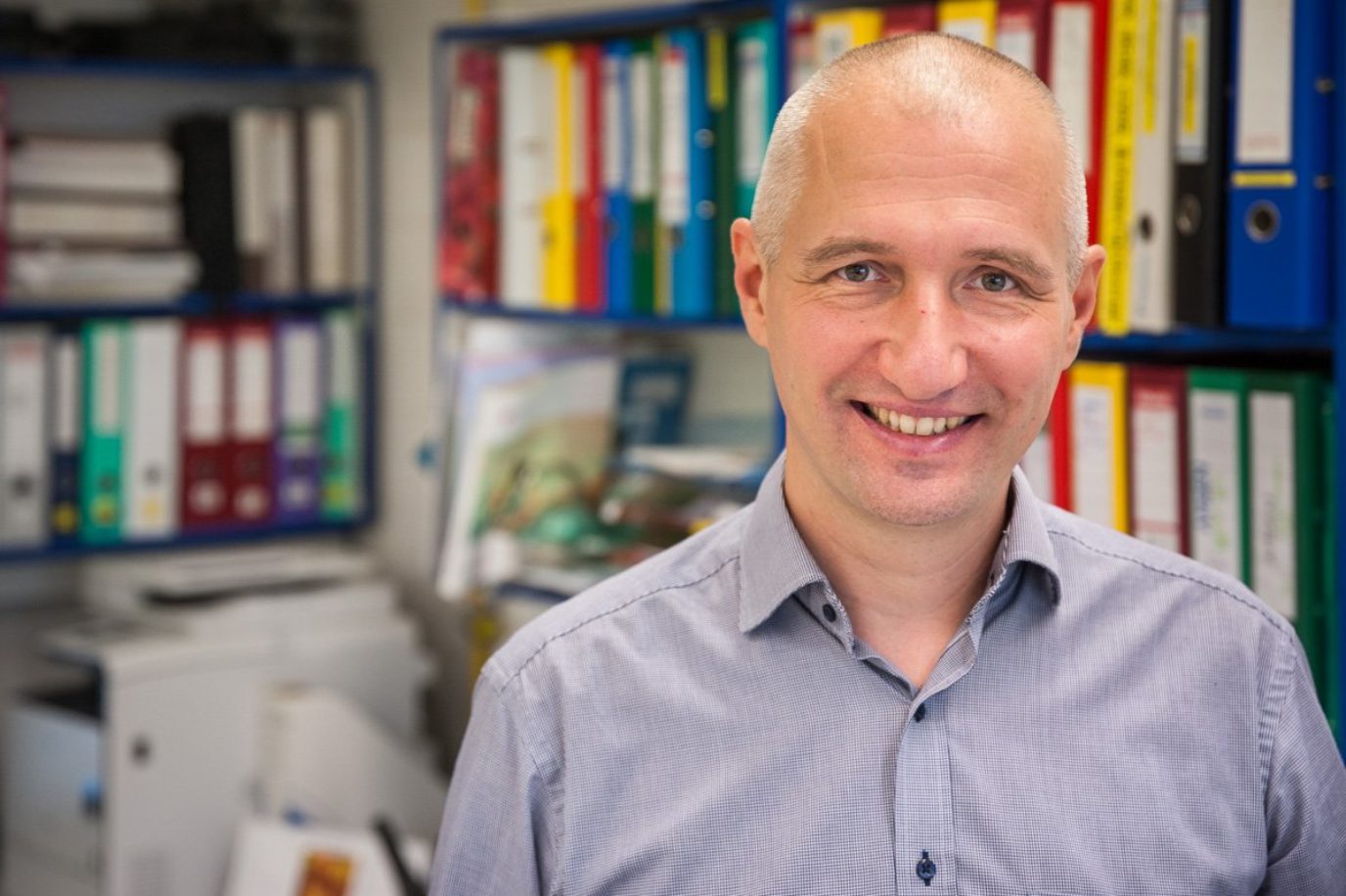
Uniquely poised between research labs and the clinic, Professor Tomáš Kalina and his team at the Charles University in Prague, continue to offer fascinating insights into the human immune response in real-time. As an expert in developing protocols for flow cytometry, Prof. Kalina also continues to strive for the standardization of methods of hybridoma generation for diagnostic applications, so crucial to this field. Standardization, argues Prof. Kalina, will be essential for the incorporation of precision medicine into our current clinical practices.
- ProteoGenix: Can you tell us about your academic and professional journey? What inspired you to devote your career to immunology?
- Throughout your career, you have used and developed immunomonitoring technologies for clinical investigation and diagnostics. In what circumstances are these technologies more advantageous than conventional approaches to monitor disease progression?
- Otherwise, what are the other conventional tools for diagnostics in these cases?
- You are continuously developing new procedures and approaches (polychromatic, spectral, and mass cytometry) for immunomonitoring. At this moment, which of these approaches could be more easily adapted for large-scale clinical diagnosis? And why?
- Are these immunotechnologies currently employed for clinical monitoring in hospitals?
- How do you think we could leverage these technologies even further? What do you think it’s still hindering its more widespread use in clinical settings?
- In your opinion, what are the most important characteristics of monoclonal antibodies and panels of antibodies used for this type of application?
- So, you believe buyers and vendors of the antibodies are still speaking “different languages” when it comes to validation?
- This need to educate users stems from the fact that these characteristics may determine how much time you spend optimizing a specific panel?
- What type of analysis should be mandatory to ensure that these molecules meet the necessary standards?
- For these assays, do you typically use IgG monoclonal antibodies? How are these antibodies produced?
- What steps can manufacturers take to ensure the highest possible quality of these reagents?
- Speaking of clinical monitoring, many promising therapeutic candidates fail to reach clinical efficiency. Do you think we could improve their chances of getting clinical approval by co-developing them alongside the use of immunomonitoring tools?
- Throughout your career, what has been your most surprising finding?
- Tell us more about other exciting projects happening at your lab.
- What do you think will be the greatest breakthroughs in clinical diagnosis in the coming decades?
- Further information
ProteoGenix: Can you tell us about your academic and professional journey? What inspired you to devote your career to immunology?
Professor Tomáš Kalina: As a medical student, I became fascinated with immunology because it provided explanations for many molecular events that often lead to disease. For me, it was enthralling to see how the theoretical concepts of molecular biology and cellular interactions affected real people and translated into real diseases.
By coincidence, during my studies, I also started working in a laboratory that implemented flow cytometry quite early. In this lab, I had a chance to observe and measure the key players of our immune system and see for myself how they acted during hematological malignancies and immunodeficiencies.
This experience has forever influenced my career choices. From that moment onward I’ve decided to devote some years of my life to clinical research by using cytometry was my main tool. Interestingly, at the time, I thought I would eventually resume my medical career, but after 19 years in this field, this still has not happened. Today, I still enjoy working with cytometry to phenotype, count cells, and, more recently, to evaluate the immune cell system in a more holistic manner.
Throughout your career, you have used and developed immunomonitoring technologies for clinical investigation and diagnostics. In what circumstances are these technologies more advantageous than conventional approaches to monitor disease progression?
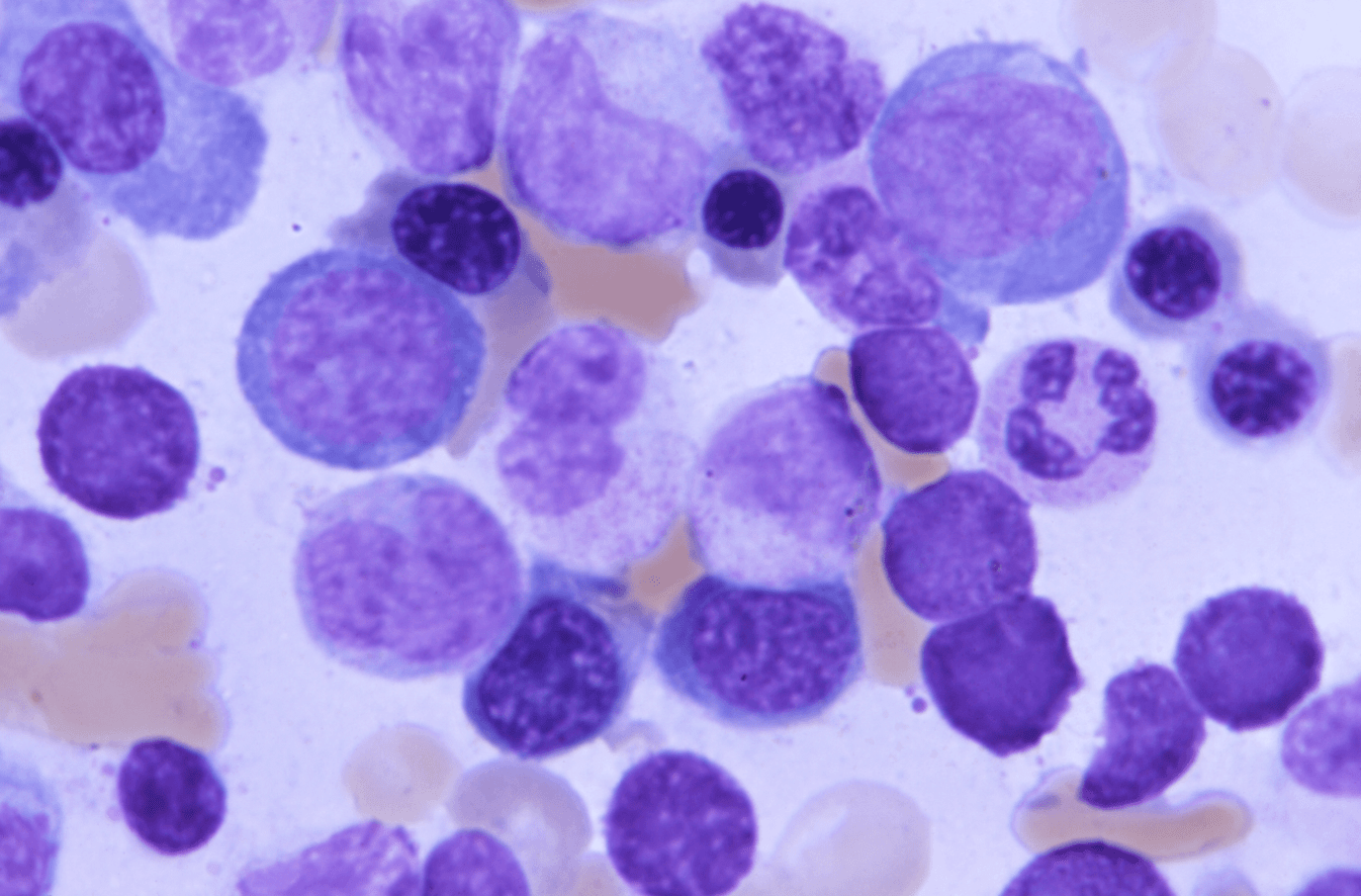
Over the years, I’ve been involved in the design, development, and validation of diagnostic methods that employ flow cytometry to either monitor hematological malignancies in children (i.e. leukemia or lymphoma) or to detect primary immunodeficiencies occurring at a very young age or later in life (e.g. severe combined immunodeficiency and common variable immunodeficiency, respectively).
The advantage of using flow cytometry for diagnosing these conditions lies in its fast turnover during sample processing and its high resolution. But the beauty of the technique also lies in its simplicity. We can receive a sample from a patient and provide an answer on the same day. This is especially important when we’re dealing with acute leukemia or severe combined immunodeficiency, where clinicians need to take immediate action to ensure their patients have the best chances of surviving the disease.
Otherwise, what are the other conventional tools for diagnostics in these cases?
Until the 1980s, these diseases were diagnosed using microscopy and histological methods. But because white blood cells don’t have a striking morphology, these techniques couldn’t deliver very strong conclusions.
Under the microscope, white blood cells looked white, round, and unremarkable. It was only when monoclonal antibodies came into use that we were able to disclose how heterogeneous and exceptional this population was.
Today, with the rise of genetics and genomics approaches, these techniques became complementary and sometimes necessary to back up the antibody-based diagnosis. They are very informative but suffer from long turnover times, and even fast assays may take more than 2 days to produce an accurate diagnostic.
You are continuously developing new procedures and approaches (polychromatic, spectral, and mass cytometry) for immunomonitoring. At this moment, which of these approaches could be more easily adapted for large-scale clinical diagnosis? And why?
All methods have some pros and cons. Essentially these methods form a spectrum from those that offer a very large sample throughput to those that offer a very broad and deep insight into the cellular immunophenotypes. The latter can make use of many markers through mass cytometry or spectral cytometry approaches. They offer a high level of resolution and are well-amenable to standardization, making them suitable for robust and in-depth clinical investigation.
On the contrary, for large-scale clinical diagnostics and big clinical monitoring studies we need methods with a high sample throughput like polychromatic flow cytometry. At the moment, clinical polychromatic flow can handle 8 to 12 markers per cell type. We achieve that combining a set of monoclonal antibodies into well-defined panels and we’re using those panels for diagnosis.
However, our limitation to 12 markers may change in the next 5 years, as antibody developer shift from developing single antibodies into developing ready-made or nearly ready-made panels, and as more powerful instrumentation becomes widely available.
Are these immunotechnologies currently employed for clinical monitoring in hospitals?
These technologies are used in clinical diagnosis since the 1990s, but it was only after the year 2000 that we started measuring more than 6 markers in a single analysis.
Moreover, it was only recently that we became able to clinically measure 8 to 12 markers across multiple labs with reproducible results, allowing us to deliver the necessary depth for monitoring even very rare marker subsets.
How do you think we could leverage these technologies even further? What do you think it’s still hindering its more widespread use in clinical settings?
Historically, we were limited by the instrumentation and by the number of fluorophores we could use in one assay. But this is not the case anymore, as the last decade brought us ground-breaking developments in this field. With the advent of polymer dyes and the development of state-of-the-art equipment, we can now combine 30 or more different fluorophores in a single assay.
Currently, our challenges are more of a logistical and practical nature: how can we cost-effectively build large and robust panels?
This turned out to be quite complicated, due to the current gap between antibody providers and the final users. Partially due to regulations, vendors usually provide single-color reagents and users prepare their specific panels independently.
Unfortunately, this is not very practical nor useful as it hinders the implementation of specific panels across multiple labs. Thus, I believe it is urgent to close this gap. We can do that by encouraging antibody developers to provide panels of reagents instead of single reagents. This would make clinical diagnostics using flow cytometry more robust and easily implemented across different hospitals and labs.
Another practical hurdle hindering the implementation of these techniques is the data. As we add more markers to a single assay, we are also exponentially increasing the amount of data we generate in a single assay. We can now measure not hundreds nor thousands, but a hundred thousand different cells from a single sample. This produces information that needs to be deconvoluted and interpreted.
At the moment, many bioinformatics and computational methods are being developed to understand and interpret this information, however, we’re still lagging in terms of implementation.
In your opinion, what are the most important characteristics of monoclonal antibodies and panels of antibodies used for this type of application?
Monoclonal antibodies are great reagents. Yet, when it comes to flow cytometry applications, we are still in urgent need of proper and thorough validation. Unfortunately, we are also still lacking a universal definition of proper antibody validation. And I believe that if we solve this issue, we’ll be driving this technology towards a more established and widespread implementation.
For this to happen, users need to ask for a more thorough characterization. We need to know if the antibody we’re purchasing is monospecific, i.e. it won’t cross-react with other targets relevant to our analysis. Moreover, we need to ensure that the antibodies we’re using are reliable, robust, and easily validated by measuring quantifiable characteristics.
As users, if we understand exactly what we’re buying, we have better chances of developing successful antibody panels. The more information we have on a specific antibody, the less the variables we need to assess or optimize during the troubleshooting phase.
In some sense, we’re not yet speaking the same language when it comes to validation, so, it will take work and time to change that.
So, you believe buyers and vendors of the antibodies are still speaking “different languages” when it comes to validation?
That’s one line of potential conflict. But this conflict also extends to different users across different hospitals and labs.
In general, users still have a very fragmented knowledge on how to select the best reagents for their studies. For this reason, we need to build more trust in these applications by educating users on how to select an antibody, based on their properties.
All antibodies on the market today have been validated in one way or another. However, the criteria used for their validation is typically hidden. This happens when antibodies are generated using proprietary technologies, or even when users disregard the importance of this information, which can be seen by many as overwhelming or unnecessary.
This need to educate users stems from the fact that these characteristics may determine how much time you spend optimizing a specific panel?
That’s one reason. But what is even more important is that if there’s any sort of poor performance in terms of cross-reactivity or lack of reactivity, researchers may be generating false results without being aware of that.
When researchers use antibodies that cross-react with unrelated targets, this can cause the contamination of the scientific literature by producing findings that are misleading or simply not reproducible.
Conceptually this is very difficult to deal with because this mistake is very difficult to disclose or troubleshoot. You may have many studies across independent labs leading to the same conclusions, but if they all used an antibody that cross-reacted with an unrelated target, those conclusions will be misleading instead of informative.
What type of analysis should be mandatory to ensure that these molecules meet the necessary standards?
In a nutshell, we need to know the actual nature of the antibodies. Ideally, the ID of the clone used to generate the antibody would allow us to compare the findings of the different research groups. Information about antibody selectivity and cross-reactivity would also need to be disclosed. And, more importantly, we would also need to know how the affinity of a specific antibody is affected by different assay conditions.
This is especially important because there is no universal protocol for staining the cells prior to analysis. If you want to stain 4 intracellular targets in a given sample, you need to fix the cells and permeabilize the membranes to make sure the antibody reaches its target. The problem is that multiple antibodies will have different performances based on the protocol used for cell fixation and permeabilization.
For this reason, each antibody should be characterized by a number of different protocols. Only then will we be able to set up multicolor panels under the same conditions that would be working reliably and robustly.
Finally, antibody developers should be more precise in terms of the intensity of staining of different fluorophore conjugates. Each individual reagent contributes with its signal to the overall signature of a particular cell, for this reason, if we want to use bioinformatics to compare datasets between different patients, we need to ensure there is no fluctuation of the signal between different studies and different patients.
This is relatively underappreciated in the field at the moment, and it may contribute to the increase of misleading conclusions. For this reason, I believe it’s also crucial to understand the performance of an antibody intensity-wise, this would allow for a more robust comparison between different samples and patients.
For these assays, do you typically use IgG monoclonal antibodies? How are these antibodies produced?
For flow cytometry, we typically use IgG mouse monoclonal antibodies generated in different clones. At the moment, there are thousands of different clones available and this number is constantly growing as more clones are produced by antibody developers. This leads to a relatively large portfolio to choose from, but it can also create confusion in the final users who struggle to make an informed decision.
Perhaps, soon these reagents will start to be produced as recombinant proteins. However, this would add another layer of difficulty, because although recombinant proteins are well-characterized, the nature of the original clone is not often disclosed. This can cause further identity issues and difficulties in translating the findings from one study using the original clone to other studies using recombinant reagents.
What steps can manufacturers take to ensure the highest possible quality of these reagents?
I think it’s essential that we, as users, work together with the manufacturers to understand what information needs to be made available about each reagent.
Characteristics such as the identity of the original clone, antibody production and conjugation method, and antibody affinity under different conditions, should be made available for available. In a nutshell, it would be ideal to build a comprehensive performance benchmarking for each reagent.
This is something that we are working on in the scope of the Human Cell Differentiation Molecules (HCDM) council that I am involved with. At HCDM we are building a resource that shows the performance of different antibody-based reagents. Our observations have led to the creation of a public database that serves to help both vendors and users of this technology.
Speaking of clinical monitoring, many promising therapeutic candidates fail to reach clinical efficiency. Do you think we could improve their chances of getting clinical approval by co-developing them alongside the use of immunomonitoring tools?
My team and I have been involved both in research studies and in immunomonitoring for clinical evaluation of therapeutic antibodies. More recently, we have also been involved in the clinical evaluation of cell-based therapies such as CAR-T.
We noticed that the focus of most initial studies is the drug itself. In the early stages, researchers seldom pay attention to how the response to a specific treatment is modulated by the cellular context in actual patients.
In these early stages, researchers are not leveraging the speed and resolution of flow cytometry for clinical evaluation. For this reason, I do agree that a careful and robust immunomonitoring approach could contribute with much precise information that would guide the efforts during antibody development.
For instance, if you are targeting inhibitory molecules and you try to block its effect, you need to know whether the cells responsible for the production of these molecules are present at relevant concentrations in the patient you are trying to treat. If those cells are not there or if they are there but do not express the inhibitory molecule, most likely, your targeted therapy is not going to change anything in the immune system of that specific patient.
I do feel that sometimes there was not enough attention being paid to the context. Because of this, assumptions were made that didn’t apply to all cohorts of the study.
For this reason, using flow cytometry during clinical evaluation might increase our understanding of how a specific treatment works, but it might also increase the effectiveness of these therapies by determining which patients best respond to a given drug.
Throughout your career, what has been your most surprising finding?
I was always fascinated by the fact that we are able to build an approach that allowed us to capture the complexity of our immune system.
For instance, we have worked in mass cytometry with human B cell development in the bone marrow. It’s really fascinating when you are able to see and track the complete development of the B cell from the stem cell throughout all the progenitor stages, all the way to the mature naïve B cell and then follow its journey to the periphery. We can see the entire journey simply by taking snapshots from either normal donors or from patients who have any sort of disease that alters the development of these cells.
After all these years, it still surprises me how much we can gain from a single evaluation.
Tell us more about other exciting projects happening at your lab.
I’m still really focused on developing a more precise understanding of the different immunophenotypic and functional changes that occur in patients suffering from primary immunodeficiency caused by a single gene defect.
This is a program where we are fortunate to collaborate with other groups of clinicians who are working with these patients in their outpatient departments. In these cases, the clinicians provide us the samples and we provide them a fast and reliable diagnostic, that is often validated by our colleagues responsible for the genetics studies. If these studies reveal a new type of mutation, or if they reveal a mutation with a new consequence, we can study the effect of this single-gene mutation on the patient’s immune system in real-time. This is what makes me really thrilled these days.
We also have an ongoing project with the HCDM where we are continuously working on remapping all the known monoclonal antibodies that were ever assigned a CD (cluster of differentiation) which, at the moment, comprises nearly 400 different antibodies. By doing so, we want to establish their expression levels across all cell types in the peripheral blood.
This will help us not only to improve the way we design new flow cytometry assays, which a very specific application, but it will also help us to understand the potential side-effects of therapies that target some of these CDs.
If we extend this concept to pediatric leukemia, which is my current field of work, we will potentially find new targets or targetable proteins that are expressed in leukemic cells and, thus, can be used as markers of new targeted therapy. We can use flow cytometry to ensure that these targets are exclusive for the leukemic cells and are not present in a normal hematopoietic cell.
What do you think will be the greatest breakthroughs in clinical diagnosis in the coming decades?
In the next decade, we will probably witness the rise of more integrative approaches. We will not only understand the molecular defects but also measure its effects on the human immune system and individual blood cells.
The integrated insight will enable us to either repair or block different pathways using targeted therapies and close the clinical loop by measuring the response to these therapies through immunomonitoring. By closing the loop we’ll be bringing the concept of precision medicine to everyday practice. The implementation of immunomonitoring for clinical evaluation and diagnostics will also help us understand which patient should receive which drug, and whether that patient will profit from the drug. Since we will be able to measure the response in real-time, we’ll be able to adjust the therapy to the patient’s unique immune system.
Further information
The HLDA11 Workshop, the 11th workshop organized by Prof. Pablo Engel and his colleagues at the HCDM, is serving to assign new CD and names to groups of so far unassigned monoclonal antibodies that target G protein-coupled receptors (GPCRs).
They are receiving submissions from both academic groups and industrial partners actively engaged in the development of antibodies. These submissions will serve as a multi-laboratory blind analysis of monoclonal antibodies that is set to validate the specificity and usability of these precious reagents. Thus, reestablishing the trust of users and helping standardize the use of flow cytometry as an efficient tool for clinical research and diagnostics.
More information about the current workshop can be found at: http://www.hcdm.org/index.php/hlda11-workshop
- Kalina, T. Reproducibility of Flow Cytometry Through Standardization: Opportunities and Challenges. Cytometry A. 2020; 97(2):137-147. doi: 10.1002/cyto.a.23901
- Kalina, T. et al. Relevance of Antibody Validation for Flow Cytometry. Cytometry A. 2020; 97(2):126-136. doi: 10.1002/cyto.a.23895
- Kalina, T. et al. CD Maps—Dynamic Profiling of CD1–CD100 Surface Expression on Human Leukocyte and Lymphocyte Subsets. Front Immunol. 2019; 10:2434. doi: 10.3389/fimmu.2019.02434
- Flores-Montero, J. et al. Fluorochrome choices for multi-color flow cytometry. J Immunol Methods. 2019; 475:112618. doi: 10.1016/j.jim.2019.06.009