 Antibody production
Antibody production
Mastering Hybridoma Technology: The Future of Monoclonal Antibodies in Research and Medicine
Scientists and researchers in fields spanning from healthcare and biotechnology to agricultural sciences have long sought reliable methods to produce highly specific and consistent antibodies. Imagine you are a researcher aiming to develop a monoclonal antibody that targets a unique protein implicated in a novel viral infection. You believe that this antibody could revolutionize diagnostics and therapeutics, potentially saving countless lives. But there's a challenge. Creating a highly specific monoclonal antibody involves isolating and producing a single type of antibody from a vast repertoire of immune cells, a task that could take years if not decades to achieve through traditional methods. What if there was a proven, efficient way to generate these monoclonal antibodies with high specificity and affinity? A technique that could produce these essential tools for research and medicine reliably and at scale? Hybridoma technology is the answer to this challenge. Developed in the 1970s, this groundbreaking method allows scientists to create immortal cell lines capable of producing monoclonal antibodies indefinitely. Hybridoma technology has since become the backbone of antibody production, facilitating numerous advancements in medical diagnostics, therapeutics, and biotechnological research. This blog post is your comprehensive guide to hybridoma technology. We will delve into its principles, methodologies, clinical applications, and the latest advancements. Whether you're new to the field or looking to deepen your understanding, this encyclopedia of hybridoma technology will provide you with the insights and knowledge you need. Let's begin.
- Brief Overview of Hybridoma Technology
- Importance and Relevance to Researchers and Scientists
- History and Development
- Historical Context
- Origins and Early Developments in Hybridoma Technology
- Key Milestones in Its History
- Introduction to Hybridoma Technology
- Definition and Overview
- Step-by-Step Guide on Hybridoma Development
- Hybridoma Cells
- Characteristics and Types of Hybridoma Cells
- Types of Hybridoma Cells
- Generation and Culture of Hybridoma Cells
- Clinical and Practical Applications
- Monoclonal Antibody (mAb) Therapeutics
- In Vivo Diagnostics
- Immunotherapy
- Biotechnological Advancements
- Benefits and Limitations of Hybridoma Technology
- Benefits
- Limitations
- Challenges and Advancements in Hybridoma Technology
- Current Challenges
- Recent Advancements
- Future Prospects
- Monoclonal Antibody Production
- Overview of Monoclonal Antibodies
- Key Advantages of Hybridoma Technology for Monoclonal Antibody Production
- Enhance Your Hybridoma-Based Antibody Discovery with ProteoGenix
- Boost Your Research with Our Hybridoma Services
- Why Choose ProteoGenix for Your Hybridoma-Based Antibody Discovery?
- Start Your Hybridoma-Based Antibody Discovery Journey with ProteoGenix
- Conclusion
Brief Overview of Hybridoma Technology
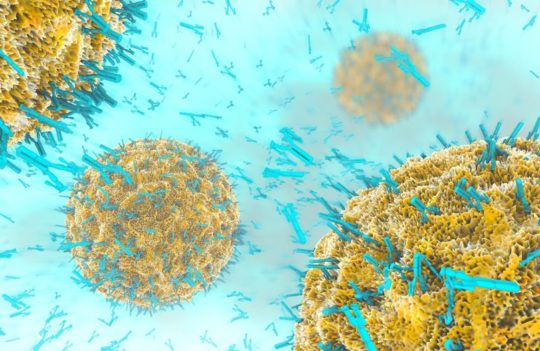
Hybridoma technology is a revolutionary technique used to produce monoclonal antibodies (mAbs) by fusing a specific type of immune cell with a cancer cell. This fusion results in hybrid cells, known as hybridomas, that combine the longevity and rapid division of cancer cells with the antibody-producing capability of immune cells. Hybridomas can be cultured indefinitely, allowing for the continuous production of large quantities of identical antibodies, which are crucial for various applications in research, diagnostics, and therapeutics.
Importance and Relevance to Researchers and Scientists
Hybridoma technology holds immense significance for researchers and scientists, particularly those involved in the fields of immunology, biotechnology, and medical diagnostics. Here are some key reasons why hybridoma technology is vital:
- Monoclonal Antibody Production: Hybridomas are the cornerstone of monoclonal antibody production, providing highly specific antibodies that can recognize and bind to unique antigens. These antibodies are invaluable tools in scientific research, allowing for precise targeting and study of specific proteins, cells, or pathogens.
- Clinical and Diagnostic Applications: Monoclonal antibodies produced via hybridoma technology are extensively used in clinical diagnostics and therapeutic applications. They are employed in diagnostic tests to detect various diseases and conditions, including infectious diseases, cancers, and autoimmune disorders. Additionally, monoclonal antibodies form the basis of many therapeutic agents used in treatments such as cancer immunotherapy and chronic disease management.
- Research Advancements: The ability to generate specific antibodies has propelled numerous scientific advancements. Researchers utilize hybridoma-derived antibodies in various experimental techniques, such as immunoassays, flow cytometry, and immunohistochemistry, to elucidate biological processes and disease mechanisms.
- Biotechnological Innovation: Hybridoma technology has spurred innovation in biotechnology, leading to the development of novel diagnostic tools, therapeutic agents, and research methodologies. It has paved the way for advancements in personalized medicine, targeted therapies, and biopharmaceutical development.
- Global Impact: The global impact of hybridoma technology cannot be overstated. It has transformed the landscape of biomedical research and healthcare, contributing to improved diagnostic accuracy, better disease management, and the development of cutting-edge treatments. Researchers and scientists worldwide rely on hybridoma technology to drive their work and make significant contributions to science and medicine.
History and Development
Historical Context
Origins and Early Developments in Hybridoma Technology
Hybridoma technology was pioneered in the mid-1970s, revolutionizing the field of immunology and biotechnology. The foundation for this technology was laid by César Milstein and Georges Köhler, who developed the method of producing monoclonal antibodies through cell fusion in 1975. Their groundbreaking work earned them the Nobel Prize in Physiology or Medicine in 1984.
The technique involves fusing myeloma cells (a type of cancer cell) with spleen cells from a mouse that has been immunized with a specific antigen. The resultant hybrid cells, or hybridomas, inherit the ability to produce specific antibodies from the spleen cells and the immortality and rapid proliferation characteristics of myeloma cells. This innovative approach allowed for the production of large quantities of identical (monoclonal) antibodies, which could be used in research, diagnostics, and therapy.
Key Milestones in Its History
- 1975: César Milstein and Georges Köhler introduce hybridoma technology.
- 1976: First successful production of monoclonal antibodies using hybridoma technology.
- 1980s: Widespread adoption of monoclonal antibodies in diagnostic tests and research.
- 1984: Milstein and Köhler receive the Nobel Prize for their work in hybridoma technology.
- 1990s: Development of therapeutic monoclonal antibodies for treating various diseases.
- 2000s: Advances in genetic engineering improve hybridoma techniques, increasing efficiency and specificity.
- 2010s: Hybridoma technology contributes to the development of checkpoint inhibitors and other immunotherapies.
- Present Day: Ongoing advancements in hybridoma technology continue to enhance its applications in medicine and biotechnology.
Introduction to Hybridoma Technology
Definition and Overview
Hybridoma technology is a sophisticated method developed in the 1970s for producing large quantities of identical antibodies, known as monoclonal antibodies. This process begins with the immunization of a mouse (or another mammal) with a specific antigen, triggering an immune response. Antibody-producing B cells from the spleen of the immunized mouse are then harvested. These B cells, which generate antibodies that specifically bind to the antigen, are fused with immortal myeloma cells—cancer cells that can proliferate indefinitely in vitro.
The fusion of B cells and myeloma cells produces hybrid cells called hybridomas. Hybridomas inherit the ability to produce specific antibodies from the B cells and the capacity for endless growth from the myeloma cells. This unique combination allows hybridomas to continuously produce large quantities of monoclonal antibodies, which are chemically identical, in contrast to polyclonal antibodies that are a mixture of different antibody molecules.
Hybridoma cells are cultured starting from a single viable hybridoma cell, ensuring that each culture consists of genetically identical cells producing the same monoclonal antibody. The myeloma cell line used is specifically selected for its ability to grow in tissue culture and its lack of endogenous antibody production, which ensures that the antibodies produced are solely from the fused B cells.
This technology leverages the principle that different types of animal cells can be fused to create hybridomas. The selection of cells that combine the antibody-producing capability of B cells with the long-term growth potential of myeloma cells allows for the production of unlimited quantities of any desired antibody. Monoclonal antibodies produced by hybridoma technology are essential for a wide range of applications, including research, diagnostics, and therapeutics. They are used as reagents in specific diagnostic tasks and for the purification of antigens.
Step-by-Step Guide on Hybridoma Development
The hybridoma development process involves a series of meticulously executed stages designed to produce monoclonal antibodies with high specificity and affinity:
- Antigen Design
The initial step in hybridoma development is the careful design and preparation of the antigen (Ag). An antigen is a foreign molecule capable of eliciting an immune response in the host animal. Common antigens include proteins, peptides, polysaccharides, small molecules, DNA fragments, or even entire cells. The key attributes of a desirable antigen are high immunogenicity (ability to provoke an immune response) and high antigenicity (ability to be specifically recognized by antibodies).
Antigen Selection: The antigen must be carefully selected to ensure it has high immunogenicity and antigenicity. Characteristics such as structural conformation, amino acid sequence, and accessibility significantly affect antibody binding.
Antigen Modification: For small molecules (haptens) that are poorly immunogenic, conjugation to a larger carrier protein (e.g., keyhole limpet hemocyanin (KLH) or bovine serum albumin (BSA)) may be necessary to elicit a strong immune response.
Bioinformatics Tools: Bioinformatic tools can predict and optimize antigen design by analyzing epitope specificity and ensuring the antigen will provoke a robust immune response. - Immunization of Host Animal
Once the antigen is prepared, it is used to immunize the host animal, typically a mouse. The immunization protocol usually involves multiple injections over several weeks to boost the immune response and promote the maturation of antibody-producing B cells.
Injection Protocol: Mice are often injected intraperitoneally with the antigen at intervals (e.g., day 0, day 14, and day 21) to enhance the immune response.
Use of Adjuvants: Adjuvants, such as mineral oils or aluminum salts, may be co-administered with the antigen to prolong antigen exposure and stimulate the immune system.
Immune Response Monitoring: Blood samples (test bleeds) are taken to monitor the immune response and antibody titers, ensuring the animal is producing antibodies against the antigen. - Cell Collection
Following the immunization schedule, the spleen of the immunized mouse is harvested to collect spleen cells rich in B cells. The spleen is a critical organ where B cell maturation and antibody production occur, making it the primary source of antibody-producing cells for hybridoma generation.
Spleen Harvesting: The spleen is aseptically removed from the mouse, and spleen cells are isolated using mechanical disruption and filtration to obtain a single-cell suspension.
Preparation for Fusion: The isolated spleen cells are washed and resuspended in a suitable fusion medium, ready for the next step. - Cell Fusion for Hybridoma Generation
The collected B cells are then fused with immortal myeloma cells using either polyethylene glycol (PEG) or electrofusion techniques.
PEG-Mediated Fusion: PEG is used to induce cell membrane contact and fusion. PEG dehydrates the cell membranes, causing them to aggregate and fuse. The fused cells are then washed to remove excess PEG.
Electrofusion: Electrofusion uses electrical pulses to align and fuse the cells. This method involves an initial AC pulse to align the cells, followed by a DC pulse to induce fusion, and a final AC pulse to stabilize the fused cells. - Hybridoma Selection and Screening
After fusion, the hybridoma cells are cultured in HAT (hypoxanthine-aminopterin-thymidine) medium. This selective medium ensures the survival of only the successfully fused hybridomas. Unfused myeloma cells and B cells die off in this medium due to their inability to synthesize nucleotides via the salvage pathway.
HAT Medium Selection: HAT medium contains aminopterin, which blocks the de novo nucleotide synthesis pathway. Only hybridomas, which have functional salvage pathways from the B cells, survive in this medium.
Screening Methods: Hybridomas are screened for antibody production using ELISA, flow cytometry, or other high-throughput screening techniques. ELISA detects the presence of specific antibodies in the culture supernatant. - Cloning of Hybridomas
Positive hybridomas identified during screening are cloned through limiting dilution or other cloning techniques to ensure monoclonality.
Limiting Dilution Cloning: This involves serial dilution of hybridoma cells to isolate single cells, which are then expanded into separate cultures. Each well should ideally contain one hybridoma cell, which grows to form a monoclonal population.
Expansion and Verification: Cloned hybridomas are expanded, and their monoclonality is verified by further screening to ensure they produce consistent and specific antibodies. - Expansion of Hybridomas
Cloned hybridomas are expanded in culture to produce large quantities of monoclonal antibodies.
Culture Conditions: Hybridomas are cultured in flasks or bioreactors under optimal conditions to maximize cell growth and antibody production. Factors such as temperature, pH, and nutrient supply are carefully controlled.
Scaling Up: The culture volume is gradually increased to achieve the desired antibody yield. This may involve transferring the cells to larger flasks or bioreactors. - Characterization of Monoclonal Antibodies
The produced monoclonal antibodies are characterized for their specificity, affinity, isotype, and other relevant properties.
Specificity Testing: ELISA, Western blotting, and immunohistochemistry are used to confirm the antibodies bind specifically to the target antigen.
Affinity Measurement: Techniques such as surface plasmon resonance (SPR) measure the binding affinity of the antibodies.
Isotype Determination: The antibody isotype (e.g., IgG, IgM) is determined using isotype-specific secondary antibodies in an ELISA format. - Monoclonal Antibody Purification
Monoclonal antibodies are purified from the hybridoma culture supernatants using methods such as protein A or protein G affinity chromatography.
Affinity Chromatography: Antibodies are captured on columns containing protein A or protein G, which binds to the Fc region of the antibodies. The bound antibodies are then eluted using a suitable buffer.
Concentration and Buffer Exchange: Purified antibodies are concentrated and exchanged into the desired buffer using techniques such as ultrafiltration or dialysis. - Cryopreservation of Hybridoma Cell Lines
Hybridoma cell lines are cryopreserved for long-term storage. This allows for the preservation of hybridomas for future antibody production, ensuring a consistent supply of identical monoclonal antibodies.
Cryoprotectants: Hybridoma cells are suspended in a cryoprotectant solution, typically containing dimethyl sulfoxide (DMSO) to prevent ice crystal formation during freezing.
Freezing Process: Cells are gradually frozen to -80°C before being transferred to liquid nitrogen for long-term storage.
Hybridoma Cells
Characteristics and Types of Hybridoma Cells
Hybridoma cells are unique hybrid cells created by the fusion of antibody-producing B cells and immortal myeloma cells. This fusion endows hybridomas with the desirable traits of both parent cell types: the ability to produce specific antibodies from the B cells and the capacity for endless proliferation from the myeloma cells. Here, we delve into the characteristics and various types of hybridoma cells.
- Immortality: Hybridoma cells inherit the ability to proliferate indefinitely from myeloma cells, allowing for continuous culture and large-scale production of monoclonal antibodies.
- Antibody Production: They retain the ability to produce specific antibodies from the B cells, ensuring the production of high-affinity and high-specificity monoclonal antibodies.
- Clonality: Hybridomas can be cloned to produce monoclonal populations, ensuring uniformity and consistency in antibody production.
- Versatility: Hybridomas can be engineered to produce antibodies against a wide range of antigens, including proteins, peptides, polysaccharides, and small molecules.
- Stability: Hybridoma cell lines can be cryopreserved and revived without loss of their antibody-producing capability, providing a long-term source of specific monoclonal antibodies.
Types of Hybridoma Cells
- Mouse Hybridomas: The most common type of hybridomas, derived from the fusion of mouse B cells with mouse myeloma cells. These hybridomas are extensively used for research, diagnostic, and therapeutic applications due to the well-established protocols and high efficiency of mouse immune systems in producing specific antibodies.
- Human Hybridomas: Created by fusing human B cells with human myeloma cells or heteromyeloma cells (human-mouse hybrid myeloma cells). Human hybridomas are particularly valuable for producing fully human monoclonal antibodies, reducing the risk of immunogenicity in therapeutic applications.
- Rat Hybridomas: Derived from the fusion of rat B cells with rat myeloma cells. These hybridomas are useful for producing antibodies when mouse antigens or epitopes are poorly immunogenic in mice or when cross-reactivity with mouse proteins needs to be avoided.
- Rabbit Hybridomas: Formed by fusing rabbit B cells with rabbit myeloma cells. Rabbit hybridomas can produce antibodies with higher affinity and specificity compared to mouse hybridomas, making them valuable for applications requiring highly sensitive detection.
- Other Species Hybridomas: Hybridomas can also be created from other species such as hamsters, guinea pigs, and chickens, depending on the specific needs of the research or application.
Generation and Culture of Hybridoma Cells
- Fusion Efficiency:
The efficiency of the fusion process, which combines antibody-producing B cells with immortal myeloma cells to create hybridomas, is critical for the successful generation of monoclonal antibodies. Several factors influence the fusion efficiency:
Concentration of Fusion Agents:
Polyethylene Glycol (PEG): PEG is commonly used to mediate cell fusion. The concentration of PEG must be optimized to ensure effective cell membrane fusion without causing excessive toxicity. Typical PEG concentrations range from 30-50%, with adjustments made based on the specific cell types and experimental conditions.
Electrofusion: This method uses electrical pulses to induce fusion. The parameters, including voltage, pulse duration, and frequency, must be carefully calibrated to maximize fusion efficiency while minimizing cell damage.
Temperature:
Fusion reactions are highly temperature-sensitive. Optimal temperature conditions need to be maintained throughout the fusion process. Generally, fusion is carried out at 37°C to mimic physiological conditions, which supports cell viability and fusion efficiency.
Cell Ratios:
The ratio of B cells to myeloma cells is crucial for achieving a high yield of hybridomas. A typical ratio ranges from 1:1 to 5:1 (B cells to myeloma cells). This ratio ensures that enough myeloma cells are available to fuse with the B cells, increasing the likelihood of successful hybridoma formation.
Cell Density and Viability:
High cell density and viability are essential for effective fusion. Cells should be harvested during their exponential growth phase and washed thoroughly to remove any residual serum or media components that might interfere with the fusion process.
Fusion Enhancers:
Addition of fusion enhancers, such as dimethyl sulfoxide (DMSO) or poly-L-lysine, can improve membrane fusion and hybridoma yield. These agents facilitate closer cell membrane contact and promote the fusion process.
- Hybridoma Stability:
Once hybridomas are generated, maintaining their long-term stability is vital to ensure consistent antibody production over multiple generations. Several strategies are employed to achieve this:
Cryopreservation:
Hybridoma cells are cryopreserved shortly after successful fusion and initial screening. Cryopreservation involves freezing cells in liquid nitrogen using cryoprotectants like DMSO to prevent ice crystal formation and cell damage. This process preserves the original hybridoma characteristics and antibody-producing capabilities, allowing for long-term storage and future use.
Regular Subculturing:
Regular subculturing of hybridoma cells is necessary to maintain their viability and productivity. Cells should be passaged at appropriate intervals to prevent overgrowth and nutrient depletion, which can lead to genetic drift and loss of antibody production.
Genetic Stability Monitoring:
Hybridoma cells are periodically screened to monitor their genetic stability and antibody production. Techniques such as ELISA, flow cytometry, and PCR are used to ensure that the hybridomas continue to produce high-affinity antibodies with the desired specificity.
Optimization of Culture Conditions:
Culture conditions, including media composition, temperature, pH, and oxygen levels, are optimized to support hybridoma growth and antibody production. Supplements like fetal bovine serum (FBS), amino acids, and vitamins are added to the culture media to enhance cell viability and productivity.
Mycoplasma Testing:
Regular mycoplasma testing is conducted to prevent contamination, which can affect cell growth and antibody production. Mycoplasma contamination is a common issue in cell cultures and must be promptly identified and addressed.
Antibody Characterization:
Continuous characterization of the produced antibodies ensures that they retain their specificity and affinity over time. Any changes in antibody characteristics may indicate instability or genetic drift in the hybridoma population, prompting further investigation and corrective measures.
Clinical and Practical Applications
This section explores the diverse clinical and practical applications of hybridoma technology, highlighting its crucial role in monoclonal antibody (mAb) therapeutics, in vivo diagnostics, immunotherapy, and biotechnological advancements.
Monoclonal Antibody (mAb) Therapeutics
Role of Hybridoma Technology in Developing Therapeutic Monoclonal Antibodies
Hybridoma technology has been instrumental in the development of therapeutic monoclonal antibodies. This technology allows for the production of highly specific and homogeneous antibodies, which are essential for targeted therapies. Hybridomas, created by fusing B cells with myeloma cells, can be cultured indefinitely, providing a continuous supply of antibodies against a specific antigen.
- Targeted Cancer Therapies: Hybridoma-derived mAbs are used to target specific cancer cell antigens, leading to direct cytotoxicity or immune-mediated destruction. These therapies minimize damage to healthy cells and reduce side effects compared to traditional chemotherapies.
- Autoimmune Disease Treatment: Monoclonal antibodies can neutralize pro-inflammatory cytokines or deplete specific immune cells, providing targeted treatment for autoimmune diseases such as rheumatoid arthritis and lupus.
Examples of mAb Therapeutics in Clinical Use
- Rituximab (Rituxan): Targets CD20 on B cells, used in the treatment of B-cell non-Hodgkin lymphoma and rheumatoid arthritis.
- Trastuzumab (Herceptin): Targets HER2 receptors, used in the treatment of HER2-positive breast cancer.
- Pembrolizumab (Keytruda) and Nivolumab (Opdivo): Checkpoint inhibitors targeting PD-1, used in various cancers including melanoma and non-small cell lung cancer.
- Adalimumab (Humira): Targets TNF-α, used in the treatment of rheumatoid arthritis, Crohn’s disease, and other inflammatory conditions.
In Vivo Diagnostics
Diagnostic Applications of Hybridoma Technology
Monoclonal antibodies derived from hybridomas are invaluable in diagnostic applications due to their specificity and ability to bind with high affinity to their target antigens. These antibodies are used in various in vivo diagnostic tools to detect diseases at an early stage and monitor treatment responses.
- Radioimmunodetection: Involves radiolabeled mAbs that bind to specific tumor antigens, allowing for imaging using PET or SPECT.
- Optical Imaging: Uses fluorescently labeled mAbs to visualize biological processes in real-time, aiding in disease diagnosis and research.
Examples of In Vivo Diagnostic Tools Developed Using Hybridoma Technology
- Ibritumomab Tiuxetan (Zevalin): A radiolabeled antibody used for imaging and treating non-Hodgkin lymphoma.
- Fluorescent Antibodies for Imaging: Antibodies labeled with fluorescent dyes used in various imaging techniques to study disease progression.
Immunotherapy
Application of Hybridoma Technology in Immunotherapy
Hybridoma technology is crucial in the development of immunotherapies, which harness the body’s immune system to fight diseases. Monoclonal antibodies produced through hybridoma technology are used to enhance or modulate immune responses.
- Antibody-Drug Conjugates (ADCs): mAbs linked to cytotoxic drugs, targeting cancer cells while sparing healthy tissue.
- CAR-T Cell Therapy: CAR-T cells engineered with receptors derived from mAbs to target specific cancer antigens.
- Bispecific Antibodies: mAbs that can bind two different antigens, bringing immune cells into close contact with cancer cells to facilitate targeted killing.
Examples and Case Studies of Immunotherapy Treatments
- Brentuximab Vedotin: An ADC targeting CD30 in Hodgkin lymphoma.
- Tisagenlecleucel (Kymriah): A CAR-T cell therapy targeting CD19 in B-cell acute lymphoblastic leukemia.
- Blinatumomab: A bispecific antibody targeting CD19 on B cells and CD3 on T cells, used in acute lymphoblastic leukemia.
Biotechnological Advancements
Use in Biotechnological Research and Development
Hybridoma technology has driven significant advancements in biotechnology, providing tools for protein purification, molecular biology, and drug development.
- Protein Purification: mAbs are used in affinity chromatography to isolate specific proteins from complex mixtures, essential for producing high-purity proteins for research and therapeutics.
- Molecular Biology Tools: Monoclonal antibodies are crucial in techniques such as Western blotting and flow cytometry, enabling precise detection and analysis of proteins and cell populations.
Examples of Biotechnological Advancements Facilitated by Hybridoma Technology
- CRISPR/Cas9: mAbs guide CRISPR/Cas9 complexes to specific genomic loci, enhancing gene editing precision.
- Functional Assays: mAbs are used to study the mechanisms of action of biological molecules, aiding in the development of new drugs and therapies.
Benefits and Limitations of Hybridoma Technology
Hybridoma technology has been a cornerstone of monoclonal antibody production for several decades, offering numerous advantages and some notable limitations. This section provides a balanced overview of the benefits and drawbacks associated with this technology.
Benefits
High Specificity and Affinity of Produced Antibodies
- Targeted Binding: Hybridoma technology produces monoclonal antibodies (mAbs) that bind with high specificity to a single epitope on an antigen. This precision allows for targeted therapeutic and diagnostic applications, reducing off-target effects and increasing efficacy.
- Consistent Quality: The antibodies produced by hybridomas are monoclonal, ensuring batch-to-batch consistency in antibody quality and performance, which is crucial for clinical and research applications.
Proven Technology with a Long History of Success
- Established Protocols: Hybridoma technology has been widely used since its development in the 1970s by Köhler and Milstein. It has a well-documented history of success in producing reliable and effective monoclonal antibodies.
- FDA-Approved Therapeutics: Many monoclonal antibodies approved by the FDA for therapeutic use, such as Rituximab, Trastuzumab, and Adalimumab, were developed using hybridoma technology. This track record underscores the robustness and reliability of the technology.
Ability to Produce Large Quantities of Monoclonal Antibodies
- Scalability: Hybridomas can be cultured indefinitely, providing a continuous and scalable source of monoclonal antibodies. This capability is essential for meeting the high demand in both therapeutic and diagnostic markets.
- Cryopreservation: Hybridoma cell lines can be cryopreserved, ensuring a long-term supply of specific antibodies. This allows for large-scale production as needed, with consistent quality over time.
Limitations
Time-Consuming and Labor-Intensive Process
- Complex Workflow: The process of generating hybridomas involves multiple steps, including immunization, cell fusion, screening, and cloning. Each step requires careful execution and can be time-consuming.
- Screening and Selection: Identifying hybridomas that produce high-affinity antibodies involves extensive screening and selection processes, which can be labor-intensive and require significant resources.
Potential for Hybridoma Instability
- Genetic Drift: Over time, hybridoma cell lines can undergo genetic changes that may affect their ability to produce antibodies. This instability can lead to variations in antibody quality and necessitate regular monitoring and validation.
- Loss of Productivity: Some hybridoma cell lines may lose their ability to produce antibodies after several generations, requiring the development of new hybridomas or the re-cloning of existing ones.
Ethical Considerations Regarding Animal Use
- Animal Immunization: The initial step in hybridoma production involves immunizing animals (typically mice) to generate B cells. This process raises ethical concerns related to animal welfare.
- Regulatory Requirements: The use of animals in research and antibody production is subject to stringent regulatory requirements and ethical guidelines, which can complicate the production process and increase costs.
Challenges and Advancements in Hybridoma Technology
Hybridoma technology, while foundational and revolutionary, faces several challenges and continues to evolve with numerous advancements. This section delves into the current challenges, recent advancements, and future prospects of hybridoma technology.
Current Challenges
Technical Challenges in Hybridoma Production
- Fusion Efficiency: Achieving high-efficiency fusion between B cells and myeloma cells remains a technical challenge. Factors such as the choice of fusion method (e.g., polyethylene glycol (PEG) vs. electrofusion) and optimization of fusion conditions significantly impact the success rate.
- Screening and Selection: The process of identifying hybridomas that produce high-affinity antibodies is labor-intensive and time-consuming. High-throughput screening methods are needed to streamline this process but can be costly and technically demanding.
- Hybridoma Instability: Over time, hybridoma cell lines can experience genetic drift, leading to changes in antibody production quality and quantity. Regular monitoring and re-cloning are necessary to maintain stable production.
Economic and Ethical Challenges
- Cost of Production: The production of monoclonal antibodies using hybridoma technology can be expensive, particularly in the initial stages of development. Costs associated with animal immunization, cell culture, and screening add up quickly.
- Ethical Considerations: The use of animals for immunization raises ethical concerns. Despite regulatory frameworks ensuring humane treatment, there is ongoing debate about the necessity of animal use in hybridoma production and efforts to develop alternative methods.
Recent Advancements
Technological Innovations Improving Hybridoma Efficiency
- High-Throughput Screening: Advances in automated high-throughput screening technologies, such as flow cytometry and robotic screening systems, have significantly increased the efficiency of identifying productive hybridomas.
- Microfluidics: Microfluidic platforms allow for the manipulation of small volumes of cells and reagents, improving the precision and efficiency of hybridoma production. These systems can conduct parallel screenings of thousands of hybridomas, accelerating the discovery process.
- Single-Cell Analysis: Techniques such as single-cell RNA sequencing enable the detailed analysis of individual hybridoma cells, providing insights into antibody gene expression and aiding in the selection of high-producing clones.
New Methodologies and Protocols
- Enhanced Fusion Techniques: Innovations in fusion methods, such as the use of electric pulses (electrofusion) or novel fusion agents, have improved the efficiency and consistency of cell fusion processes.
- Cryopreservation Improvements: Advances in cryopreservation techniques ensure better survival rates of hybridoma cells during long-term storage, maintaining their viability and antibody production capabilities.
Future Prospects
Emerging Trends and Future Directions
- Synthetic Biology: The integration of synthetic biology approaches could revolutionize hybridoma technology. Engineering myeloma cells to enhance their fusion compatibility and stability, or even synthesizing hybridomas de novo, could become possible.
- Alternative Hosts: Exploring the use of alternative host species for antibody production, such as transgenic animals or in vitro systems, could reduce ethical concerns and potentially improve the diversity of antibodies produced.
- Improved Animal Models: Development of genetically modified animals with enhanced immune responses could lead to the production of higher-affinity antibodies and reduce the number of animals needed.
Potential Impact on Research and Clinical Applications
- Personalized Medicine: Advances in hybridoma technology could lead to the development of more personalized therapeutic antibodies, tailored to individual patients’ needs and specific disease profiles.
- Expanded Therapeutic Areas: As hybridoma technology continues to improve, its applications could expand beyond current uses, addressing a broader range of diseases, including emerging infectious diseases and complex autoimmune conditions.
- Global Accessibility: Technological advancements may also drive down costs, making monoclonal antibody therapies more accessible globally, particularly in low- and middle-income countries.
Monoclonal Antibody Production
Monoclonal antibodies (mAbs) are highly specific antibodies produced by identical immune cells that are clones of a unique parent cell. Hybridoma technology is a pivotal method for the production of these antibodies. This section provides an in-depth look at the production process, methodologies, and protocols involved in generating monoclonal antibodies using hybridoma technology.
Overview of Monoclonal Antibodies
Definition and Importance
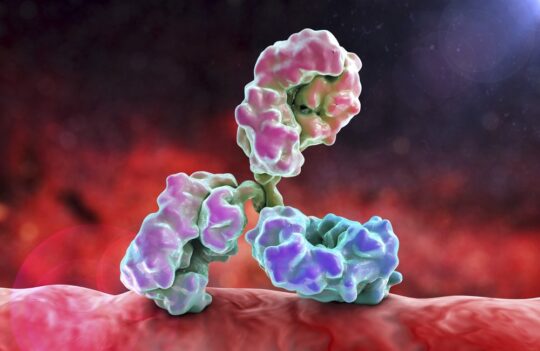
Monoclonal antibodies are uniform antibodies that target a single epitope on an antigen, offering high specificity and consistency. They are crucial tools in diagnostics, therapeutics, and research due to their ability to bind precisely to specific proteins or pathogens.
- Specificity: mAbs bind to specific antigens with high affinity, making them ideal for targeted therapies and precise diagnostic applications.
- Consistency: Produced by identical cells, mAbs ensure consistent performance in therapeutic and diagnostic applications, unlike polyclonal antibodies which are heterogeneous.
- Therapeutic Applications: mAbs are used in various therapies, including cancer treatment, autoimmune diseases, and infectious diseases, due to their ability to specifically target disease-related antigens.
- Diagnostic Applications: mAbs are essential in diagnostic tests, such as immunoassays, to detect the presence of specific biomolecules in clinical samples.
Key Advantages of Hybridoma Technology for Monoclonal Antibody Production
- High Specificity and Affinity:
Single Epitope Targeting: Monoclonal antibodies produced by hybridomas are specific to a single epitope on an antigen. This high specificity ensures precise targeting of antigens, making them ideal for both therapeutic and diagnostic applications.
Uniformity: All antibodies produced by a single hybridoma cell line are identical, ensuring uniformity in antibody structure and function. This is critical for applications requiring consistent performance.
- Immortality and Continuous Production:
Infinite Proliferation: The fusion of B cells with myeloma cells grants the resulting hybridomas the ability to proliferate indefinitely. This immortality allows for the continuous production of monoclonal antibodies without the need for repeated immunizations and cell fusions.
Scalability: Hybridoma cells can be cultured and expanded to produce large quantities of monoclonal antibodies, meeting the high demand in research, diagnostics, and therapeutics.
- Established and Proven Technology:
Historical Success: Since its development in the 1970s by Georges Köhler and César Milstein, hybridoma technology has become a well-established method for mAb production. It has been used to produce numerous FDA-approved therapeutic antibodies, underscoring its reliability and effectiveness.
Robust Protocols: The methodologies and protocols for hybridoma production are well-documented and standardized, providing a robust framework for generating high-quality monoclonal antibodies.
Enhance Your Hybridoma-Based Antibody Discovery with ProteoGenix
Boost Your Research with Our Hybridoma Services
ProteoGenix is committed to providing exceptional support for your hybridoma-based antibody discovery projects. With our comprehensive services and state-of-the-art technologies, we ensure that your research achieves optimal results. Here’s how we can assist you:
Why Choose ProteoGenix for Your Hybridoma-Based Antibody Discovery?
- Advanced Hybridoma Technology: Our expertise in hybridoma technology ensures the production of high-affinity, highly specific monoclonal antibodies. We utilize optimized protocols to maximize fusion efficiency and antibody yield.
- Comprehensive Antibody Production: From initial antigen design and immunization to hybridoma generation, screening, and antibody production, we offer a full suite of services tailored to your needs.
- Quality and Consistency: Our rigorous screening and validation processes ensure that the monoclonal antibodies we produce are of the highest quality, providing consistent and reliable performance in your applications.
- Experienced Team: Our team of skilled scientists brings extensive experience in hybridoma technology, ensuring that your project benefits from expert insights and best practices.
- Innovative Solutions: We integrate the latest advancements in hybridoma technology, including high-throughput screening, single-cell analysis, and advanced fusion techniques, to enhance the efficiency and effectiveness of your antibody discovery process.
Start Your Hybridoma-Based Antibody Discovery Journey with ProteoGenix
Partner with ProteoGenix to elevate your hybridoma-based antibody discovery project. Our dedication to quality, innovation, and client satisfaction ensures outstanding results for your research.
Ready to advance your research? Start Your Hybridoma-Based Antibody Discovery Journey with ProteoGenix
Conclusion
Summary of Key Points: Hybridoma technology is a pivotal advancement that enables the production of highly specific and consistent monoclonal antibodies, which are essential for a wide range of applications in healthcare, biotechnology, and research. This technique involves the fusion of antibody-producing B cells with immortal myeloma cells, creating hybridomas that can be cultured indefinitely to produce monoclonal antibodies. Hybridoma technology has facilitated significant progress in targeted cancer therapies, autoimmune disease treatments, and diagnostic tools. Moreover, it has driven numerous biotechnological advancements, including protein purification and molecular biology applications. Despite challenges such as production costs, technical complexities, and ethical considerations, continuous innovations are enhancing the efficiency and applicability of hybridoma technology.
Final Thoughts on the Importance of Hybridoma Technology: Hybridoma technology has profoundly impacted scientific and medical fields by providing a reliable method for producing monoclonal antibodies with high specificity and affinity. Its ability to produce consistent and scalable antibodies makes it indispensable for therapeutic and diagnostic applications. The technology’s proven success, coupled with ongoing advancements, ensures that hybridoma technology remains a cornerstone in antibody discovery and production. As new methodologies and innovations emerge, hybridoma technology’s applications and potential continue to expand, promising even greater contributions to science and medicine.
To learn more about how hybridoma technology can accelerate your research and development projects, visit our Hybridoma Services page. Our comprehensive services include antigen design, hybridoma generation, screening, and antibody production tailored to meet your specific needs. For more information, feel free to contact us directly. Our team of experts is ready to assist you in harnessing the power of hybridoma technology to achieve your scientific goals.