Antibody production
Antibody production
What makes antibody therapeutics uniquely fitted to fight autoimmune disorders?
Autoimmune disorders afflict almost 10% of the global population, with a particular incidence in young and middle-aged women. Despite the increasing diversity of autoimmune conditions, these diseases are typically characterized by an exacerbated immune response often translating into the overexpression of proinflammatory molecules (e.g. cytokines) or increased and indiscriminate activity of B and T cells. Antibody therapies for autoimmune disorders are well characterized and they mostly focus on blocking inflammation (e.g. anti-TNF antibody Utomilumab or anti-IL-6 antibody Siltuximab) or depleting autoantibody-producing B cells (e.g. anti-CD20 antibody Rituximab). What makes these therapies so successful?
The numbers and causes of autoimmune disorders
Autoimmune disorders affect 5 to 10% of the global population. But these conditions have a stronger incidence in women who are almost 80% more likely than men to suffer from these conditions. Many of these disorders are also among the top 10 leading causes of death among women above 65.
The development of treatments for cancer and autoimmune disorders are inextricably linked. They were among the first disorders ever to benefit from the development of therapeutic antibodies, and despite the widely different pathologies, many antibodies have been used interchangeably to treat the two conditions. But while cancer consists of the failure of the immune system to detect and eliminate malignant cells, autoimmune disorders are characterized by an exacerbated and overactive immune and proinflammatory response against the organism’s healthy cells and tissues.
Due to the opposite effects on our immune system, treatments for cancer and autoimmune conditions end up sharing similar targets and mechanisms of action. But while anticancer treatments aim at enhancing and redirecting the immune response to malignant cells, treatments against autoimmune disorders aim at smoothing the abnormal response. However, unlike cancer, which can be cured when detected early on, there are no curative treatments for autoimmune disorders.
Conventional antibody therapies for autoimmune disorders
Like cancer, no defined causes of autoimmune disorders have ever been described. However, experts alert to the increasing incidence of autoimmune disorders among the general population which suggests environmental and lifestyle factors may influence the development of these diseases.
Blocking the exacerbated inflammatory response caused by most autoimmune disorders is one of the most convenient ways to treat these conditions. For this reason, conventional antibody therapies for these disorders typically target either:
- Proinflammatory molecules or their corresponding receptors
- B cells, specifically CD20 and CD22 markers
- Cell-cell interactions
The key proinflammation mediators in autoimmune disorders include the cytokine tumor necrosis factor-alpha (TNF), interleukin-6 (IL-6), interleukin-1 (IL-1), and interferon-gamma (IFN-γ), which are recurrently observed in rheumatoid arthritis (RA), inflammatory bowel disease, ankylosing spondylitis (AS), and psoriasis.
Cytokines-blocking antibody therapies
TNFα-blocking antibodies such as Utomilumab, Etanercept, Adalimumab (Humira®), Infliximab, and Certolizumab were among the first antibody therapeutics ever to be found useful for the treatment of autoimmune disorders. These antibodies alleviate the inflammatory response by binding to soluble or membrane-bound TNF. Moreover, some of these molecules can cause Fc-receptor-mediated apoptosis of T cells, one of the key players across many autoimmune disorders.
Other widely useful proinflammatory blockers are anti-IL-6/IL-6R antibodies such as Siltuximab, Tocilizumab, and Sarilumab. IL-6, a well-known B cell differentiation factor, is soluble and widely expressed cytokine, while its dedicated receptor IL-6R consists of two subunits: IL-6 binding unit (80 kDa) and the membrane-bound gp130 (130 kDa) responsible for signal transduction. IL-6 is a strong inducer of acute-phase proteins (e.g. C-reactive protein, serum amyloid A, fibrinogen, hepcidin, haptoglobin, and antichymotrypsin), and exacerbated levels of IL-6/IL-6R complex are recurrently detected in RA patients and likely to contribute to osteoclast-like cell formation (joint destruction).
B cell-depleting antibody therapies
The exacerbated production of autoantibodies is well-document in several autoimmune disorders such as autoimmune blistering skin diseases, myasthenia gravis, antibody/immune-complex-mediated systemic lupus erythematosus (SLE), RA, and multiple sclerosis (MS). B cell-directed treatments known to cause B cell depletion were found to be therapeutically effective for these diseases. However, in some specific cases, B cell depletion can have the opposite effect, highlighting the need to carefully evaluate the risks before initiating a specific treatment.
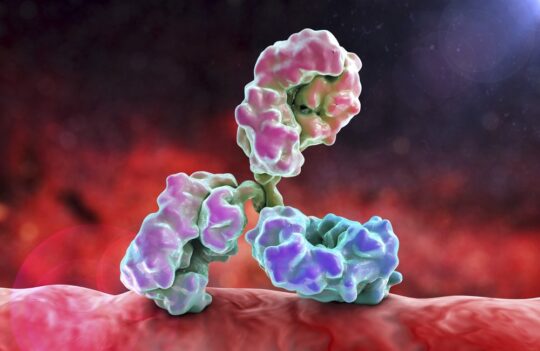
Rituximab (RTX), approved in 1997, is a chimeric human-mouse antibody designed to target the CD20 protein found on the surface of naïve and mature B cells, and absent from the surface of memory B cells. The efficiency of RTX varies widely among different patients and different autoimmune disorders, but it is well-established that this anti-CD20 treatment does not interfere with long-term immunity against vaccine-preventable diseases (e.g. tetanus, measles, rubella, etc.).
RTX was also the first anti-CD20 antibody ever to be granted FDA approval and it is still used for the treatment of multiple autoimmune conditions. By binding strongly to CD20, Rituximab mediates complement-dependent cytotoxicity against B cells which ultimately results in apoptosis and depletion of the immune cell reservoirs.
Moreover, by depleting the reservoirs of B cells, RTX can also indirectly reduce the overproduction of proinflammatory cytokines such as IL-6 and IL-7. Alternative B cell depleting therapies are currently under active development, such as human and humanized anti-CD20 antibodies or anti-CD22 antibodies, which have yet to reach the clinic.
Concluding remarks
The treatment of autoimmune disorders continues to be highly challenging because experts have yet to find the specific causes behind the onset of these debilitating diseases. However, since the discovery of the hybridoma technology and the development of antibody therapies, autoimmune disorders were among the first conditions ever to benefit from the specificity and safety of these treatments.
Antibodies are thus the ideal therapeutics to delay the devastating effects of autoimmune disorders, due to their ability to modulate our organism’s immune response. Currently, antibody therapies for autoimmune disorders specifically aim at blocking pro-inflammatory molecules or at depleting B cells responsible for overproducing autoantibodies. On occasion, these therapeutics are known to be ineffective in the treatment of specific patients or patient groups, for this reason, scientists have redoubled their efforts in developing better antibody therapies. And more effective biotherapeutics are expected to enter the market in the years to come.
- Angyal, A. et al. Application of Monoclonal Antibody Therapies in Autoimmune Diseases. Autoimmune Disorders – Current Concepts and Advances from Bedside to Mechanistic Insights. 2011. doi: 10.5772/23912
- Directorate General for Internal Policies. Policy Department A: Economic and Scientific Policy. Worshop: Autoimmune Diseases – Modern Diseases. Brussels, 25 September 2017. IP/A/ENVI/2017-09. PE 614.174. Retrieved from: https://www.europarl.europa.eu/thinktank/en/document.html?reference=IPOL_STU(2017)614174
- Hofmann, K. et al. Targeting B Cells and Plasma Cells in Autoimmune Diseases. Front Immunol. 2018; 9: 835. doi: 10.3389/fimmu.2018.00835
- Li, P. et al. Drugs for Autoimmune Inflammatory Diseases: From Small Molecule Compounds to Anti-TNF Biologics. Front Pharmacol. 2017; 8:460. doi: 10.3389/fphar.2017.00460
- Rosman, Z. et al. Biologic therapy for autoimmune diseases: an update. BMC Medicine. 2013; 11:88. Doi: 10.1186/1741-7015-11-88
- Tanaka, T. and Kishimoto, T. Targeting Interleukin-6: All the Way to Treat Autoimmune and Inflammatory Diseases. Int J Biol Sci. 2012; 8(9): 1227–1236. doi: 10.7150/ijbs.4666
- Yasunaga, M. Antibody therapeutics and immunoregulation in cancer and autoimmune disease. Semin Cancer Biol. 2020; 64:1-12. doi: 10.1016/j.semcancer.2019.06.001